While the number of Canadians being diagnosed and dying of heart disease is decreasing, heart disease is still the second leading cause of death in Canada and the number one cause of death worldwide. Twenty-nine percent of Canadian deaths per year are due to a preventable condition that we can avoid by making heart-healthy choices.
Heart and Arteries: Friends for Life
The abundance of terms related to heart disease can get confusing. Heart disease [1] is not just one condition. Many cardiovascular problems affect not only the heart’s ability to function well but also the blood vessels running throughout the body, which is why we often see cardiovascular issues in the brain, lungs and lower extremities, too.
Cardiovascular disease is an umbrella term for heart disease (including valve and rhythm issues), heart failure, diseases of the blood vessels and stroke. Coronary artery disease is by far the most common type of cardiovascular disease. Coronary artery disease is technically a disease of the arteries, the passageways that deliver—and restrict, if blocked—blood to the needy heart muscle. This disease often results in chest pain (angina) and heart attack. Another term you will often hear in this context is ischemic heart disease, which involves insufficient blood and oxygen flow to the body’s tissues.
Our Powerful Pump
Clench your fist, and there you have the approximate shape and size of your heart muscle nestled in behind your breastbone. The heart has four chambers—two upper (atria) and two lower (ventricles). Oxygen-depleted, bluish blood that has returned through the body collects in the right atrium, then flows down into the right ventricle. From there, it is pumped via the pulmonary artery to the lungs, where it picks up fresh oxygen. The now re-oxygenated, bright-red blood travels through the pulmonary veins back into the heart, but this time, it flows into the left atrium and then down into the left ventricle. Finally, it leaves the heart through the aorta to begin its next cycle throughout the body.
The heart beats an average of 100,000 times a day. Day in, and day out, from birth to death (upward of 2.5 billion heartbeats), it delivers oxygen, nutrients, hormones and other essential constituents to every cell in our body. At the same time, the blood collects cellular junk—the unwanted waste of regular processes that occur inside cells. Think of this mighty heart muscle as the pump that keeps everything else running. Just like a mechanical pump needs fuel to keep working, the heart requires a steady supply of blood and oxygen to stay healthy. Problems arise when it does not get this fuel because somewhere in the system, a blockage has occurred.
Our Artery Helpers
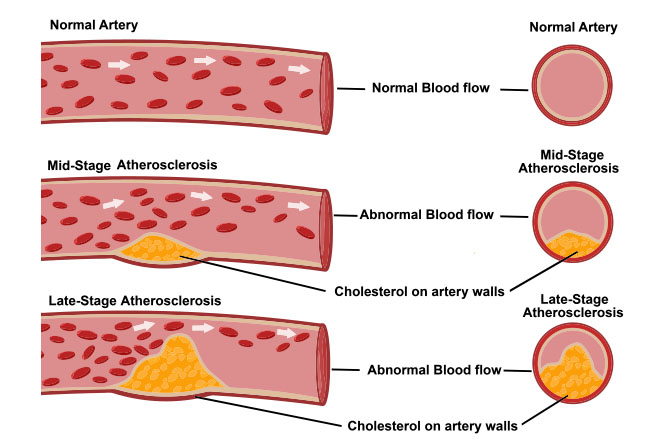
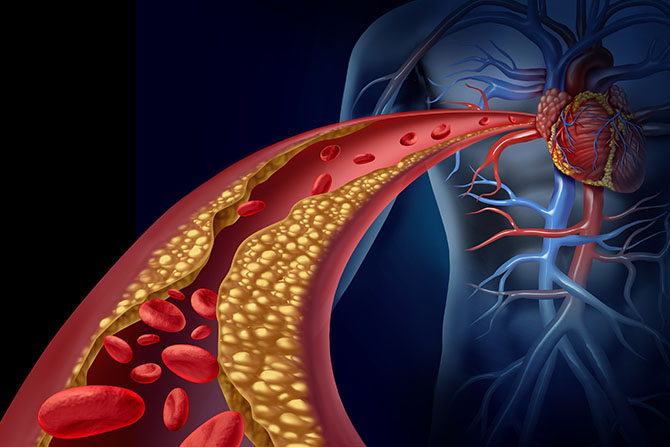
The heart has two major arteries: the right coronary artery and the left main coronary artery. Each of these arteries stretches out into smaller and smaller arteries, delivering blood deeper into the heart muscle cells. If the blockage develops in one of these arteries, we call it atherosclerosis from the Greek athere, meaning “porridge,” and sclerosis, meaning “hardening” or “scarring.” Over time, plaque builds on the arterial walls and causes them to stiffen. This accumulation narrows the arteries, and blood clots sometimes form on top of the plaque. The result is reduced blood flow through the heart. A heart attack (or myocardial infarction, meaning “death of heart tissue”) occurs if blood flow stops completely.
The most common reason for reduced blood flow to the heart is atherosclerosis. However, there are other possible reasons for blocked arteries. Blood could be too thick, for instance. Ideally, blood is thin so it can pass unheeded through increasingly tiny passageways on its way to and from cells. Sometimes, red blood cells must bend and squeeze through a single file because the arterial tunnel is so tiny! Blood thickens, and the cells clump together if the body’s clotting factors are affected. Our poor circulation then slows, and the heart is forced to work harder to counteract the effects of fatty blood.
Sometimes, the reason behind diminished blood flow lies with the heart muscle itself. Maybe it has been weakened or damaged from a previous heart attack. Or the left ventricle, which pumps freshly oxygenated blood back into the body, has been damaged by high blood pressure. The left ventricle is particularly relevant to heart disease. Uncontrolled high blood pressure can cause poor left ventricle function and worsen heart disease.
Arteriosclerosis vs. Atherosclerosis
What is the difference between arteriosclerosis and atherosclerosis? They both relate to arteries, but arteriosclerosis is any process that causes damage and hardening or thickening of our major arteries. Atherosclerosis is the most common form of arteriosclerosis and explicitly involves the nasty buildup of artery-toughening plaque. When plaque buildup happens in the coronary arteries, we get heart disease. When it happens in other parts of the body, we get impaired circulation, which can cause strokes, blood clots, and leg problems involving poor circulation, ulcers, poor wound healing, and gangrene.
Clogged Pipes
Far from being an inanimate pipe, our arteries are a player in this inner game of life. They contract and expand in response to pressure.
Arteries have three layers, the outer, tougher adventitia; the middle smooth muscle media; and an inner layer (intima) lined with a single layer of specialized cells called the endothelium. This last ultra-thin barrier is a crucial component in the development of atherosclerosis. Besides their ability to gauge blood pressure and flow, these multi-functioning endothelial cells interact with substances carried by blood, produce compounds that affect cell growth, and help govern muscle tone, thus allowing arteries to expand and contract. This expansion and contraction of arteries push blood to where it is needed.
Unfortunately, the endothelium layer frequently gets injured. The possible causes are many, including physical force and high blood pressure. Blood also carries toxins (environmental, dietary, metabolic), fatty proteins, excess blood sugar (glucose), infectious microbes and unhealthy cholesterol. These can cause endothelial dysfunction and trigger events leading to atherosclerosis, high blood pressure, heart attack, stroke, and heart failure.
The Role of Cholesterol
Cholesterol has gotten a bad rap. Our bodies produce cholesterol—a waxy, fatty substance—which performs several important functions. Cholesterol is the building block of cellular membranes and is needed to make bile acids so we can digest and absorb our food. It is also necessary to make vitamin D and hormones. To move through the bloodstream, cholesterol puts on a protective coat of lipoprotein particles: low-density lipoprotein (LDL), the “bad” cholesterol, and high-density lipoprotein (HDL), the “good” cholesterol. Generally, we want to keep LDL cholesterol levels down to prevent it from lodging in arterial walls. Conversely, we want higher HDL cholesterol levels, which protects the heart by sweeping LDL cholesterol through the arteries towards the liver. Here it is processed, then excreted from our system.
When endothelial cells are damaged, they trigger an immune response. The body sends in a repair team to address the inflamed injury, but other scroungers also show up: blood fats and bad LDL cholesterol. Now, rather than help with repairs, immune cells begin an overzealous inflammatory process. As they migrate into the artery wall to help the injury, they ingest the LDL cholesterol and form bloated, fatty foam cells that form atherosclerosis plaque. The damage is worse if the LDL cholesterol is oxidized, i.e., previously damaged by free radicals. Oxidized LDL cholesterol also damages neighboring cells at the injury site in a chain-reaction-type effect.
Free Radicals and Antioxidants
Think of rust for a minute. Slowly, various chemical reactions occur resulting in an invasive corrosion that is the bane of every vehicle owner’s existence! The damage created by free radicals in the body is like rust.
Free radicals are a natural byproduct of everyday reactions that produce energy for the body. Other major sources and generators include:
- Eating fried foods, oils heated over their smoking point, and rancid fats
- Eating nitrates and nitrites in meats
- Toxic airborne chemicals
- Cigarette smoke, or smoke from forest fires
- Exposure to medical or electromagnetic radiation (i.e., computer terminals)
- Excessively strenuous exercise
- Drinking chlorinated water
- Eating a high-fat diet
- Eating processed foods
- A diet high in sugar
- Prolonged physical and/or emotional stress
Many free radicals are highly toxic, mutagenic (cause cells to mutate), and carcinogenic (cause cancer). What these tiny molecules lack in size, they make up in destructive capacity. Stable molecules are held together by two electrons, but free radicals are missing one electron they attempt to steal from neighboring molecules. Such molecular theft causes an undesirable ripple effect where other molecules in cells and cell membranes are damaged, and more free radicals are formed. Eventually, if left unattended, what was once comparable to a spot of rust becomes a car riddled with unsightly holes.
Antioxidants are free radical scavengers. They readily disable free radicals, preventing healthy body tissues from being damaged. When the body is deficient in antioxidants, our risk of disease increases, and aging accelerates. The progression of free radical damage can, fortunately, be kept in check with antioxidants from our food and nutritional supplements.
By eating foods rich in antioxidants such as vitamins A, C, and E, selenium and phytochemicals (the pigments that give plants their colors), we can keep our defences against free radicals strong and stave off their heart-unfriendly effects. Supplemental pycnogenol, sytrinol and coenzyme Q10 serve the same important function, and further protect against heart disease.
When Plaque Ruptures
As atherosclerosis progresses, the arterial plaque grows and hardens as more cholesterol is absorbed into the artery wall, other fats, and inflammatory cells. A cap form over this. Some are big; some are small. Smaller plaques are more dangerous because they have a greater tendency to rupture in response to a variety of physical and emotional triggers. When this plaque ruptures, the immune system erroneously orders the production of factors that dissolve the plaque cap, causing its contents to spill back into the artery. Another immune response kicks in, attracting blood platelets. They clump together around the ruptured plaque and, along with red blood cells and other clotting factors, form a blood clot. A heart attack results if that blood clot entirely blocks a coronary artery.
How tragic that the first symptom of heart disease to be taken seriously is usually a heart attack and, sometimes, death.
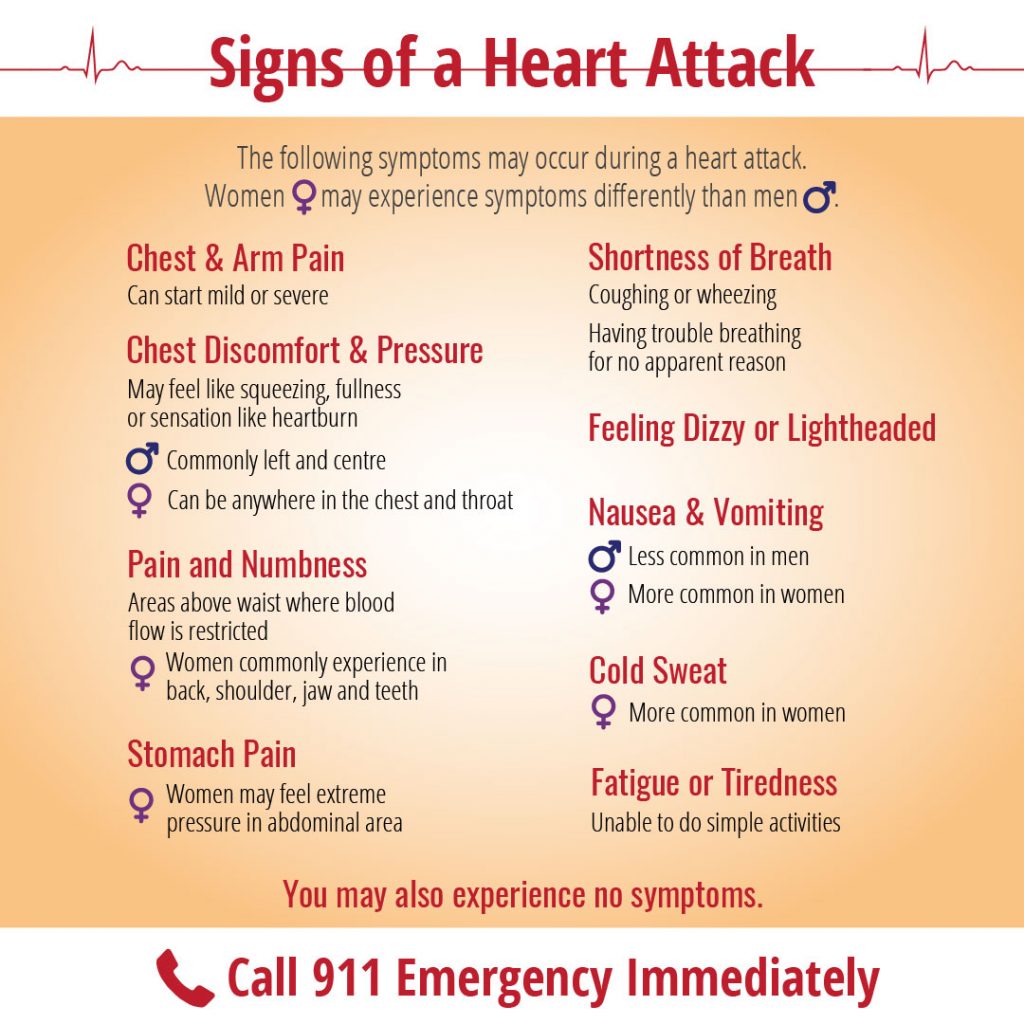
The problem often lies in our general disconnect from our bodies. We are under such stressors in daily life that we miss or disregard many warning signs like chest pain, which occurs when coronary arteries narrow by about 50 percent. Medically termed angina (Latin for “squeezing of the chest”), symptoms include:
- Pain radiating from the chest that spreads to your left arm, neck, back, throat or jaw
- Tightness, pressure, squeezing and/or aching in your chest or arm(s)
- Persistent sensation of moderate to severe indigestion
- Sharp, burning or cramping pain
- An ache starting in, or spreading to, your neck, jaw, throat, shoulder, back or arm(s)
- Neck or upper back discomfort, particularly between the shoulder blades
- Numbness in your arms, shoulders or wrists
Women with angina are more likely to notice abdomen, shoulder and back discomfort than men. Likewise, with actual heart attacks, symptoms vary between the sexes.
In the case of a heart attack or symptoms leading up to it, the quicker medical attention is sought, the greater the chances of avoiding heart damage. The longer the blood supply is impeded or cut off, the more damage the heart potentially sustains. After 20 to 40 minutes, damage can be irreversible. Living tissue becomes scar tissue.
When women get a diagnosis and treatment, it usually occurs when they are older, and heart disease is more advanced. Sadly, women are more likely to brush off bouts of warning signs, perhaps fearing embarrassment. Women are also more likely than men to drop out of cardiac rehabilitation programs after a heart attack.
Other Heart Conditions
Arrhythmias
Usually, the heart beats 60 to 100 times per minute with the same lapse between each beat. Arrhythmia represents an irregular rhythm. There are several types of arrhythmias which vary in degrees of risk. Some are linked to underlying heart disease, others to low thyroid, iron deficiency, anemia, magnesium deficiency, and stress.
Ventricular tachycardia and ventricular fibrillation are potentially fatal. In atrial fibrillation, which occurs in one percent of people over the age of 60, the heart seems to quiver instead of beating regularly because electrical impulses have been disturbed. If the underlying cause is treated, an arrhythmia will often settle down on its own.
Valve Disorders
With mitral stenosis, the heart’s mitral valve has a narrowed opening that restricts blood flow from the left atrium into the left ventricle. Shortness of breath results when blood pressure builds up in the atrium and affects the lungs. If the valve develops a leak, blood flows backward into the heart chamber, requiring the heart to work harder and, over time, possibly resulting in heart failure. Causes include mitral valve prolapse, infectious bacteria or a damaged heart muscle.
In aortic stenosis, a narrowed aortic valve reduces blood flow from the heart to the rest of the body. The left ventricle enlarges due to the strain, possibly resulting in angina or faintness. If left unrepaired by surgery, congestive heart failure and death may result. The aortic valve can also develop a leak, eventually causing heart failure if untended.
Heart Failure
When the heart muscle is weak, damaged and/or abnormally thick, it becomes an inefficient pump. The result is insufficient blood flow to the body that leads to heart failure. As the body tries to compensate, symptoms include a higher heart rate, increased blood pressure and fluid retention. As the current population living with heart disease rises, so does the incidence of heart failure. Acute heart failure occurs when the heart suddenly stops pumping efficiently. Blood backs up in the pulmonary veins, and the pressure causes the lungs to fill with fluid (pulmonary edema), creating an emergency situation.
The most common cause of heart failure is coronary artery disease, which usually occurs after one or more heart attacks and resultant high blood pressure. Other causes include valvular heart disease, inflammatory viruses and diseases, and damage caused by alcohol and drug use. Symptoms include swelling (edema) of the legs, feet or abdomen, shortness of breath, a nighttime cough, fatigue, chest pain and pressure, weight gain and dizziness. Keep in mind that not everyone with progressive heart failure exhibits symptoms.
Interestingly, we now know that heart failure differs between the sexes. In men, it is usually due to systolic dysfunction, meaning that the heart is weakened, enlarged and cannot sufficiently pump blood throughout the body. This is often referred to as a “floppy heart”. Women, meanwhile, have what is described as a “stiff heart” that is associated with what is known as diastolic dysfunction, meaning that the heart’s ability to relax between beats is impaired. A stiff heart muscle is small and cannot fill normally with blood. Regardless of whether your heart is floppy or stiff, heart failure is treatable and should be monitored.
Prevention is Best
The expression “Prevention is a pound of cure” applies to no condition better than to heart disease. By taking proactive steps to address those risk factors we can change, we can stave off or even avoid intrusive conventional medical treatment and reduce the need for medications. A multidimensional approach to heart health greatly improves our quality of life, and helps return our focus to the things that matter most in our lives.