Are you at risk? Too many people are unaware of their risks for developing cardiac illnesses. But there are known factors that should be assessed and monitored. Below we cover the recommended health tests to assess your heart health.
Cholesterol, the Good and the Bad
Few substances as controversial as cholesterol, and no substance about which there is more confusion. We need cholesterol, yet it can also play an undesirable role in atherosclerosis. When small injuries or nicks occur in the arteries, cholesterol, which acts as an internal Band-aid, can get out of control and, with the help of other factors, clog arteries and increase our risk of heart attack and heart damage.
“Bad” LDL cholesterol contributes to heart disease. But it can be kept in line by “good” HDL cholesterol, which helps sweep LDL through the body and also helps prevent LDL from oxidizing. Oxidized LDL causes plaque formation, inflammation and damage to neighboring cells. As if this were not enough, there are very low density lipoproteins (VLDL) to watch out for. These extra-small bad cholesterol particles are more likely to both form arterial plaques and oxidize due to free radical damage. People with lots of smaller LDL particles have a higher risk of heart disease than those with larger LDL particles.
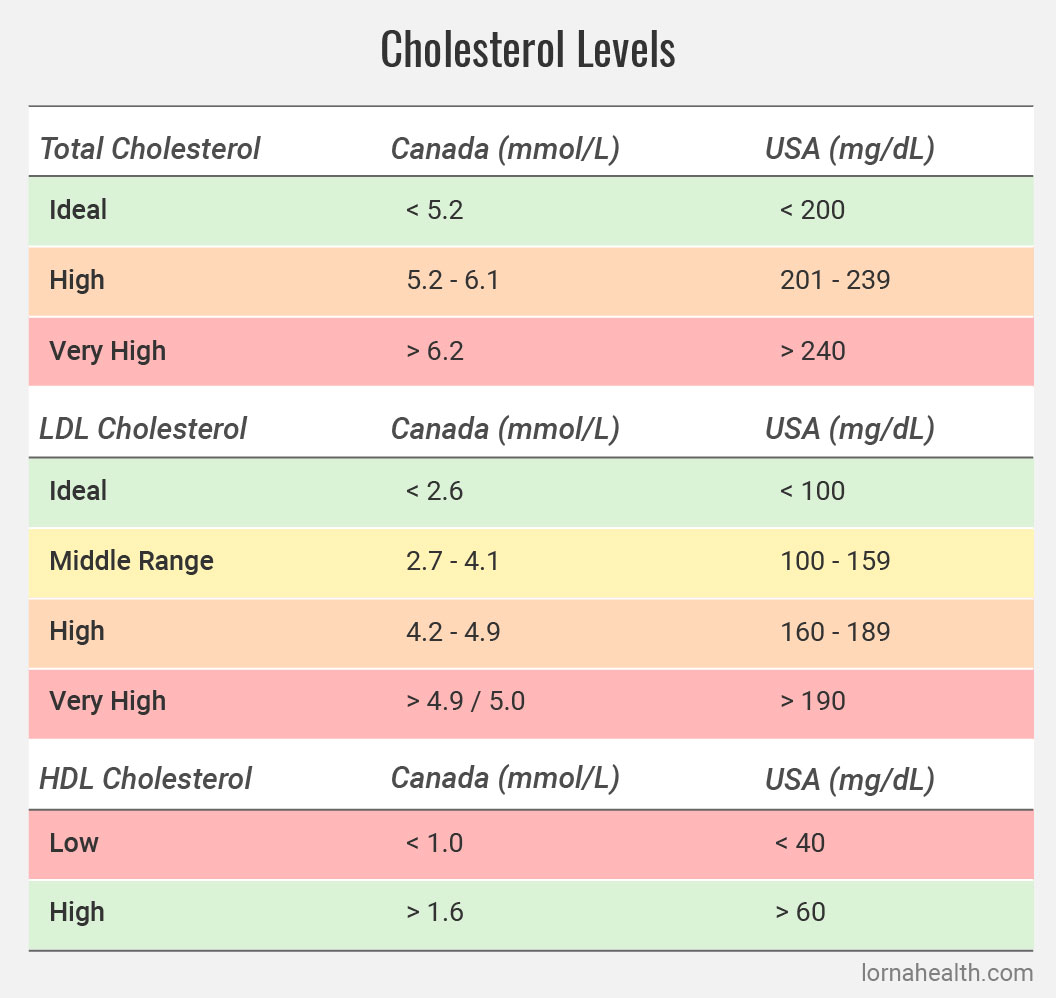
About 40 percent of North Americans have higher than recommended cholesterol levels, although it is important to keep in mind that “recommendations” continue to evolve along with our understanding of the mechanisms behind heart disease. Traditionally, it was believed that your total cholesterol measure (derived by adding LDL and HDL levels together) was the best predictor of heart disease risk. It is now held that the ratio of total-to-HDL cholesterol is more accurate. For people with zero or one risk factor for developing heart disease in the next 10 years, a ratio of 6:1 is considered acceptable. However, if you are at moderate or higher risk of developing heart disease with two or more risk factors — the category into which most people fall — maintaining a lower ratio through diet, lifestyle, supplements and fitness is very important. Generally, the lower the ratio the better, with an ideal ratio being about 4:1. Dr. Julian Whitaker, author of Reversing Heart Disease, suggests a desirable total-to-HDL cholesterol ratio of less than 3:1.
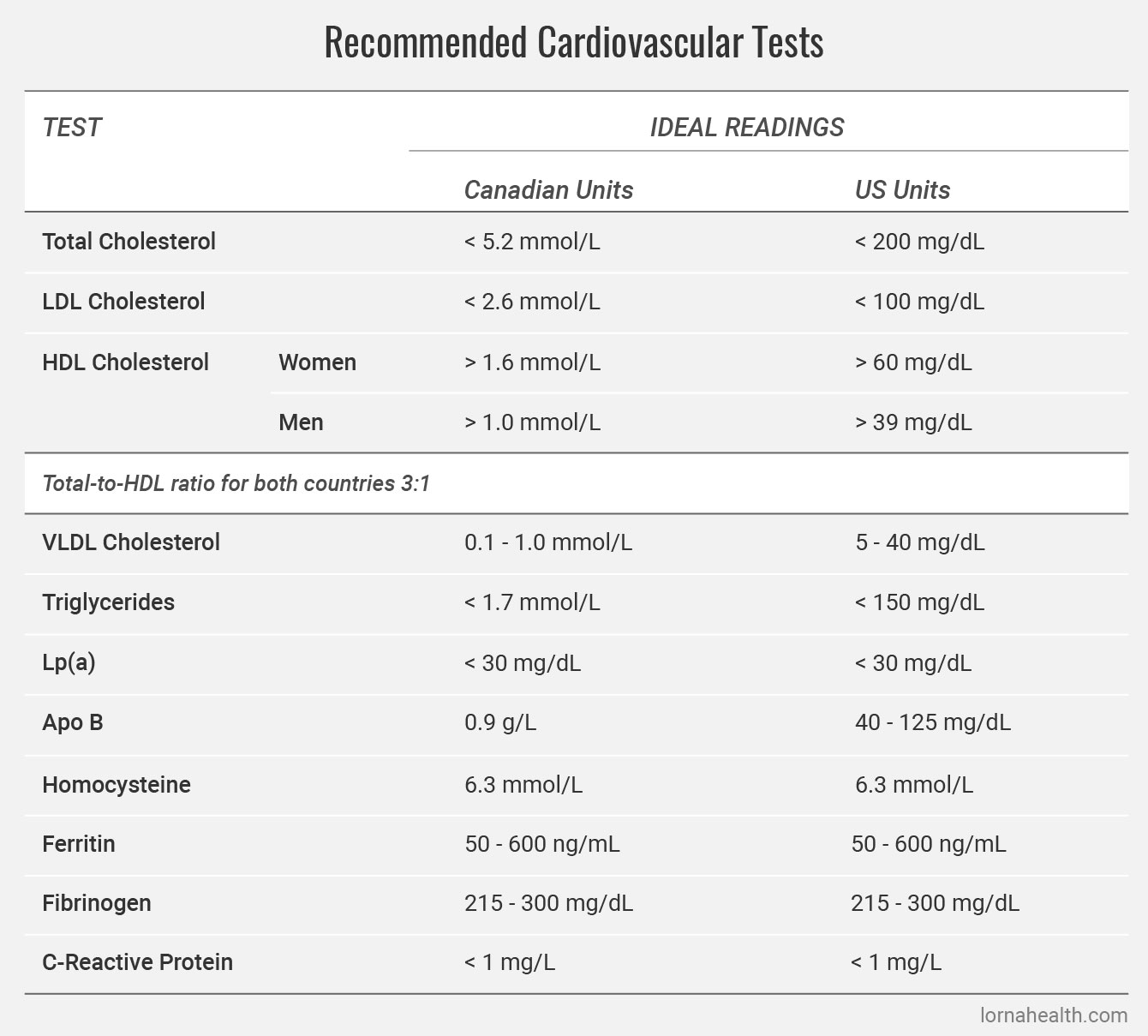
The traditional cholesterol test that has been used for decades gives readings for LDL, HDL and triglycerides, but not for newer heart disease indicators. You may require a specialized test requisitioned through your health-care provider. The newer VAP cholesterol test is very comprehensive and likely to catch on in medical testing circles although still relatively unused in North America. The VAP test categorizes LDL cholesterol by size, identifies HDL subclasses (some of which are more heart-protective than others), measures very low density lipoprotein (VLDL), and more. It is valuable to know your VLDL reading as another marker in your lipid (fat) profile. A “normal” VLDL reading is 5-40 mg/dL (0.1-1.0 mmol/L).
Good Cholesterol
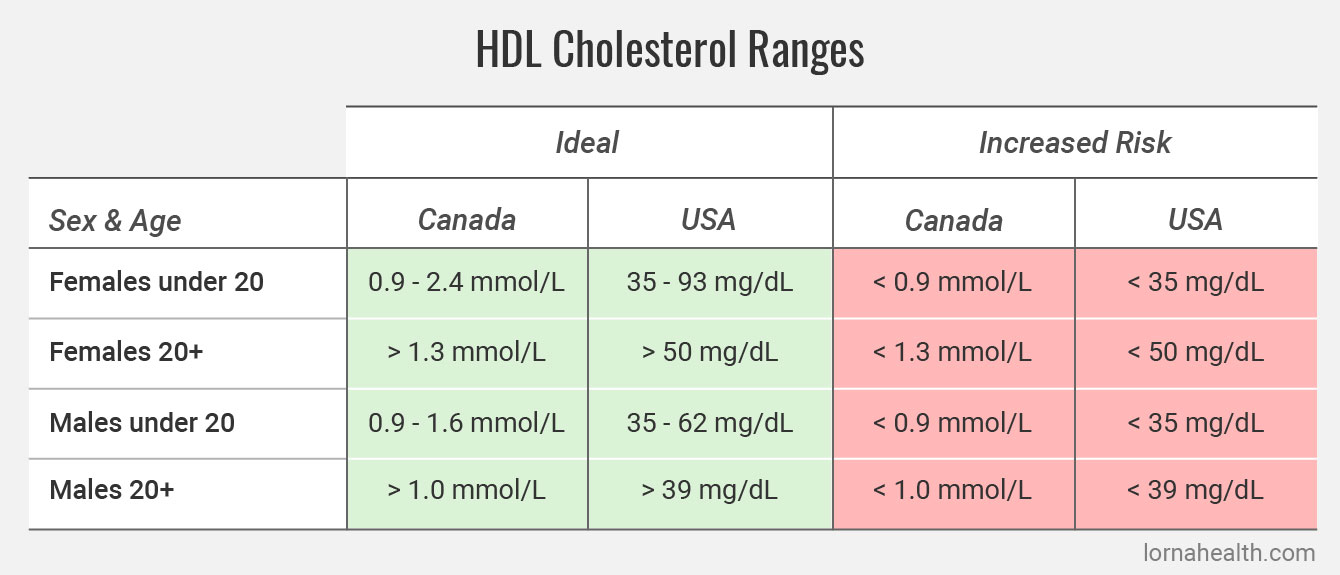
HDL is particularly relevant to women. For women, having low HDL is ever more of a risk factor than having high “bad” LDL. Even small decreases in HDL cholesterol after menopause significantly increase the risk of heart disease. In fact, HDL cholesterol is so protective that a low amount is considered an independent risk factor for heart disease.
Maintaining a healthy cholesterol profile is very achievable. Nine out of 10 people can lower high LDL, lower VLDL and improve HDL with dietary changes and nutritional supplements alone. Only 10 percent of people will require medication to keep levels in check. This is probably a shock to most people, considering that cholesterol-lowering statins are the number one prescribed drug in North America and that every time official “recommended” cholesterol levels drop (as they have several times), millions more North Americans are encouraged to take pharmaceuticals to lower LDL.
This raises a point to consider. How low is too low when it comes to LDL?
Some research indicates that LDL may serve more of a physiological purpose than previously thought. Researchers reported in the Canadian Medical Association Journal last year that “LDL cholesterol levels below 2.8 mmol/L [108 mg/dL] and levels of at least 3.9 mmol/L [150.9 mg/dL] were both associated with markedly elevated risk of cancer.” This study examined type 2 diabetics, who are prime consumers of statin-lowering drugs due to the link between diabetes and heart disease.
Another fact pointing to the need to question current cholesterol assumptions is that many heart attack victims have “normal” cholesterol levels. This has been noted in numerous studies, including a 2009 study that looked at almost 137,000 Americans hospitalized for heart attacks between 2000 and 2006. Seventy-two percent had cholesterol levels suggesting that they were not at risk of cardiovascular disease. Many people who have heart attacks also have what is considered normal blood pressure. Clearly, another silent force is at work. Cholesterol is not the universal bad guy, and although cholesterol is a factor in heart health, it is not the only factor. Rather, cholesterol should be considered as part of a complete cardiovascular health assessment.
Triglycerides
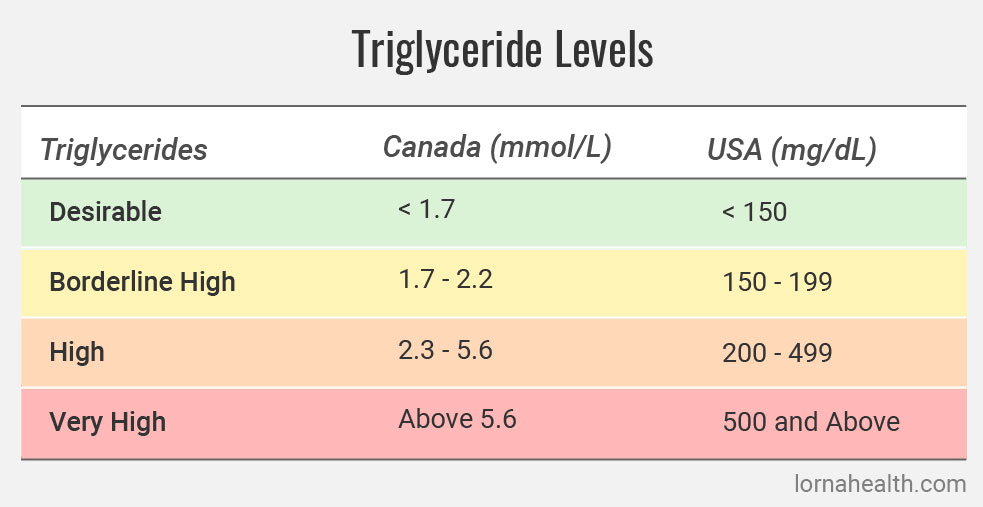
Like cholesterol, triglycerides are a blood fat. They are the most common form in the body and are manufactured in the liver. When we eat too many high-calorie, high-sugar foods (or drinks) and our body cannot burn the energy off fast enough, blood triglyceride levels shoot up and we store the triglycerides as fat. (Grab that extra roll around your middle—you’re grabbing triglycerides.) Triglycerides slide through the bloodstream on the very low-density lipoprotein (VLDL) cholesterol particles that contribute to atherosclerosis and instigate free radical damage.
Elevated triglyceride levels increase our risk of heart disease and are linked to diabetes and prediabetic syndromes, such as syndrome X. Insulin resistance, which underlies all these metabolic conditions, essentially prompts the liver to produce more VLDL, which raises triglyceride levels. This fatty blood grows sluggish while its ability to carry oxygen is reduced.
Fortunately, like cholesterol, triglycerides are very responsive to diet and lifestyle modifications and the nutritional supplements.
Lipoprotein(a) and Apolipoprotein B
Lipoprotein(a), or Lp(a), is a type of LDL cholesterol that is indicated in increased heart disease risk. One 2000 British review of 27 studies found that patients with elevated Lp(a) had a 70 percent increased risk of heart disease. Lp(a) is thought to hinder the ability to dissolve blood clots, thus increasing heart attack risk. Lp(a) also plays an inflammatory role in atherosclerosis and/or detrimentally affects the thickness and responsiveness of the arteries.
Apolipoprotein B (Apo B) is found in the VLDL and LDL particles that cart cholesterol through the blood. This small, dense protein binds with receptors on cells, promoting our uptake of cholesterol. Knowing your Apo B reading can help determine the type and/or cause of a high cholesterol reading.
Testing for Lp(a) and Apo B is less common but still available through blood work requisitioned by your doctor. If you are deemed “at risk” for cardiovascular disease, it may be covered by health-care plans. The VAP test can also detect them, although VAP testing, will likely be an out-of-pocket expense.
Normal values for Lp(a) are less than 30 mg/dL in the U.S. and 0.8 mmol/L in Canada. For Apo B, the normal level is 40-125 mg/dL and a recommended 0.9 g/L respectively.
Homocysteine: Too Much of A Good Thing
To build and repair tissues and muscles, the body uses methionine, a protein. A byproduct of this repair process is the amino acid homocysteine. Unnaturally elevated levels of homocysteine in the blood damage the endothelium cells in the arteries and promote atherosclerosis. Homocysteine also stimulates abnormal growth of smooth muscle in the middle layer of the arteries, which can then thicken the wall and clog the artery in question. Homocysteine can also promote blood clots by stimulating the body’s clotting mechanisms.
Elevated homocysteine triples the risk of heart attack, even after all other risk factors are accounted for. In 1997, the Journal of the American Medical Association reported that a high total homocysteine level represents an independent risk factor for heart disease similar to that of smoking or high blood fats (cholesterols, trigycerides). It also powerfully increases the risk associated with smoking and high blood pressure.
Fortunately, the body has a built-in mechanism for dealing with too much homocysteine. We need adequate amounts of folic acid and vitamins B6 and B12 to support methylation, which converts homocysteine into harmless elements. People who are deficient in these nutrients have high homocysteine levels. We can achieve adequate levels of B vitamins through a proper diet and by taking a good multivitamin containing B vitamins, thus supporting homocysteine reduction pathways and reducing our risk of heart attack.
There is no universal “normal” or “safe” range of homocysteine, which is measured by a blood test in mmol/L. You will hear doctors say 5-15 mmol/L is standard. Most people are about 10 mmol/L, which is also the therapeutic target recommended by the American Heart Association. A typical cardiovascular risk profile ordered through a naturopathic doctor sets the range at 3.0-14.0 mmol/L. Any reading above 6.3 mmol/L is associated with a steep increase in heart attack risk so the lower end of the scale is a better target to aim for.
Ferritin
Iron is needed for hemoglobin, a protein in the red blood cells that deliver oxygen throughout the body. We also need iron for energy, muscle tone and healthy organ function. While many people, especially vegetarians and the elderly, are at risk for iron deficiency, too much iron is an important marker of cardiovascular health. Ischemic heart disease, iron overload and hemochromatosis (an inherited disorder where the body cannot store iron properly) are associated with high levels of ferritin, a protein in cells that stores iron so the body can use it later. Those with excessive levels of iron will need to donate blood.
A ferritin test indirectly assesses how much iron is stored in the body.
The serum (blood) ranges are:
- Men: 15–410 ug/L
- Women: 15–247 ug/L
Ideal levels are above 50, and below 600.
The lower the reading (ug/L), the greater the likelihood of iron deficiency. Symptoms include fatigue, weakness, lack of stamina, poor concentration, headache, hair loss, pallor, irritability and a craving for ice.
Iron deficiency anemia [1] also has a negative affect on heart health. Because anemia leads to a decrease in blood oxygen, to make up for this the heart has to pump more blood. Low iron can lead to an enlarged hear, irregular or rapid heart beats.
Fibrinogen: Blood Clot Indicator
Without the blood’s ability to stop bleeding, even the smallest cut or scrape would be life-threatening. When a blood vessel breaks, chemical messengers and clotting factors hurry to plug the injury, then convert the liquid in the vicinity into a thicker clotty gel. One of these clotting factors is fibrinogen, produced by the liver. Although fibrinogen levels rise as we age, even in healthy people, the effects of too much fibrinogen in the body is of growing interest in the field of cardiology.
The Stress Factor
Could fibrinogen be the explanation for the clear link between stress and heart disease? The results of a very interesting 2005 Belgian study suggest so. The researchers questioned whether factors such as job stress, job control and social support impacted chronic inflammation and infection in the body. They found that, in 892 Belgium men, job stress was associated with increased fibrinogen, even after considering other factors such as age, job type, body mass index, use of medications for cholesterol and blood pressure, smoking and alcohol consumption.
High levels of fibrinogen put us at increased risk for blood clots and, ultimately, heart attack (as most heart attacks are caused by blood clots that form in arteries clogged by atherosclerotic plaque). A blood clot can also break away and travel via the bloodstream to lodge elsewhere. Following a heart attack, excess fibrinogen is a marker for increased mortality.
According to a 2005 Italian study that followed for 42 months 92 men who had suffered heart attacks, after taking into account all other factors such as age, body mass index, blood pressure, smoking and blood lipids (fats), fibrinogen levels were the only independent predictor of death. It has also been shown to be an independent marker for overall and cardiovascular mortality in patients with end-stage kidney disease, and as a marker for the silent brain vessel lesions that increase stroke risk.
A large 2005 meta-analysis in the Journal of the American Medical Association noted “moderately strong” associations between usual plasma fibrinogen level and the risks of coronary heart disease, stroke and other vascular mortality.
Fibrinogen tests can be ordered by your doctor, or purchased online through various direct-to-consumer companies. According to the US National Institutes of Health, a “normal” fibrinogen range is 200-400 milligrams per deciliter (mg/dL) of blood. The Life Extension Foundation suggests optimal fibrinogen levels are between 215-300 mg/dL. The reference ranges on a typical naturopathic cardiovascular test profile are 175-425 mg/dL. Your reading should be considered within the context of your complete cardiovascular assessment profile.
C-Reactive Protein: Inflammation Agent
Inflammation is your immune system’s first reaction against infection or injury. When a thorn cuts through the skin on your finger, damaging tissue and allowing invaders like bacteria into your body, your immune system goes to work immediately, sending out many different types of specialized cells, each with their own action.
The injured area often becomes hot, red, swollen and painful. The heat is produced by the increased blood flow to the injured area. Redness occurs because the battle and repair processes are underway. And the area usually becomes swollen because of all the fluid and immune cells at the site. Pain is often the first indicator of inflammation. It makes you take notice and stop moving the affected area to prevent further injury.
Inflammation is an effective way of ensuring that invaders do not enter your body and create havoc, but when it becomes low-grade and chronic, your immune system’s army stays revved up and damages healthy tissues in the crossfire. Scientists are realizing that this life-saving process, designed to ward off bacteria, viruses and parasites, creates disease when it’s left unchecked. It leads to the painful and damaging inflammation that attacks joints, organs or arteries.
Inflammation is a major factor in heart disease. It is the suspected reason why a surprisingly high percentage of people who have had a heart attack nevertheless have normal cholesterol and blood pressure. Even in people with normal blood cholesterol, occasionally cholesterol finds its way into the lining of the arteries and is embedded there as plaque. (Those with high blood cholesterol are at greater risk of this happening.) Our immune response causes inflammation that triggers the eruption of these plaques and the formation of blood clots that silently set the stage for heart attacks.
C-reactive protein (CRP) is produced by the liver during an inflammatory response. In a large-scale Harvard study involving 540 physicians, men with the highest CRP levels were three times more likely to have a heart attack and twice as likely to have had a stroke than men with the lowest levels. One year later, in 1998, a study looked at C-reactive protein in women. This inflammatory marker beat out cholesterol levels as a predictor of heart attack or stroke. “Women who developed cardiovascular events had higher baseline CRP levels than control subjects… Those with the highest levels of CRP had a 5-fold increase in risk of any vascular event and a 7-fold increase in risk of [heart attack] or stroke.” Women using hormone replacement therapy have to be aware that estrogen (Premarin was the brand used in the studies) increases inflammation in the body and elevates CRP to dangerous levels, indicating a much higher risk of heart attack and particularly strokes.
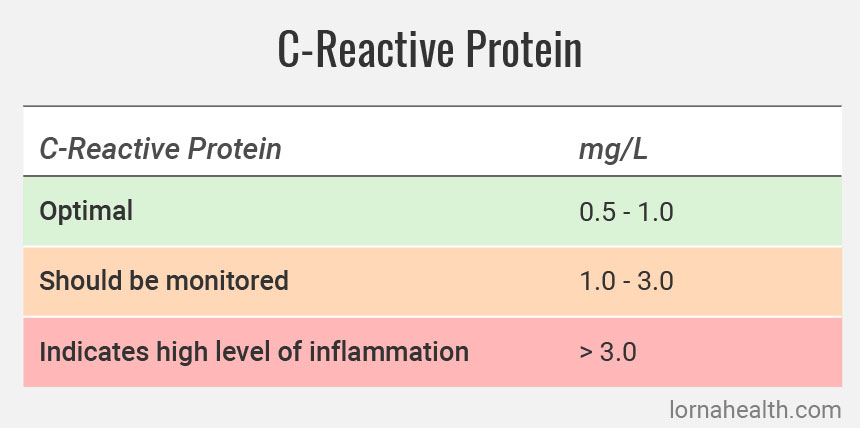
The amount of CRP in the blood is a good indicator of how much inflammation is occurring anywhere in the body, including in the arteries. Ask your physician for a high-sensitivity CRP (HS-CRP) blood test. If you have a CRP level over 3.0 mg/L, you should following be a heart-smart diet and nutritional supplementation [2] program to reduce CRP quickly.
High Blood Pressure (Hypertension)
With this common condition that affects one in three Americans and one in five Canadians, the heart muscle contracts too forcefully and sends blood driving through the body with excess force. Clogged arteries can create additional resistance that causes damage in the sensitive inner endothelium layer. This “wear and tear” promotes additional plaque buildup that leads to heart disease. People with high blood pressure are more than twice as likely to have a heart attack compared to people with normal blood pressure. Hypertension also strains and eventually weakens the heart, while very high blood pressure can cause blood vessels to burst in the brain, causing stroke.
Systolic vs. Diastolic
A blood pressure reading has two parts, systolic pressure (the top number) and diastolic pressure (the bottom number). The higher systolic reading represents the pressure just after your heart beats (i.e. when your heart contracts and pushes blood out into arteries). The lower diastolic reading is the pressure while your heart is at rest, refilling with blood between beats.
The ideal adult blood pressure reading is less than 120/80, measured in millimeters of mercury (mmHg). High blood pressure is considered anything higher than 140/90.
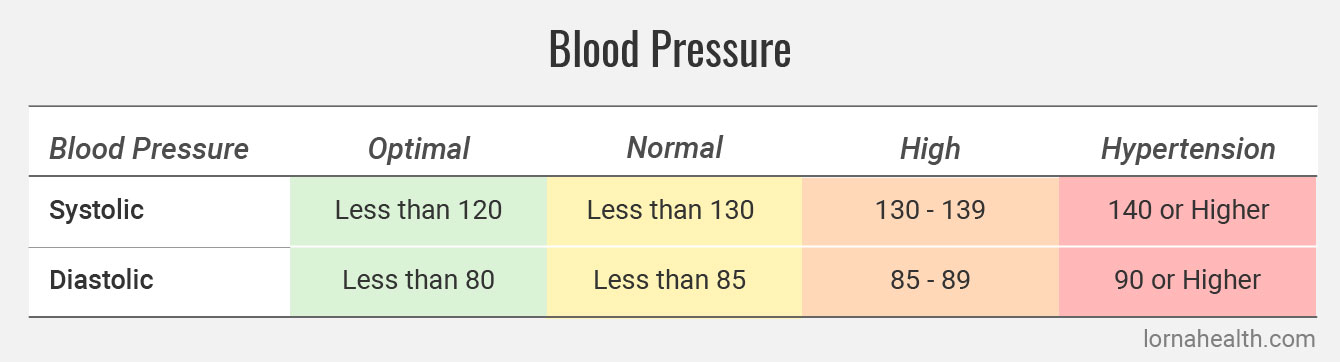
A new category of high blood pressure called “prehypertension” category is between 130-139/85-89 mmHg. Sixty percent of us with prehypertension will graduate to hypertension within four years unless we make heart-healthy diet, fitness, and lifestyle changes designed to bring our blood pressure back down. Even a 1 mmHg drop in diastolic blood pressure can shrink your risk for heart disease by two to three percent.
Have your blood pressure checked regularly. High blood pressure generally does not cause overt symptoms; one-fifth of Americans and two-fifths of Canadians do not know they have it. Like heart disease, blood pressure abnormalities respond well to non-invasive, non-medicated methods of intervention.
Causes of High Blood Pressure
- Age (blood pressure can increase with age)
- A poor diet
- Magnesium deficiency
- Too much alcohol
- Lack of exercise
- Obesity
- Stress
- Another health condition, e.g. kidney disease or thyroid dysfunction (both more common in women than men)
- Pregnancy
- Birth control pills and hormone replacement therapy (HRT) use
- Certain drugs, e.g. amphetamines (stimulants), diet pills and some cold and allergy pills
Recommended Cardiovascular Tests
Below is a full list of all recommended tests and their ideal ranges: