There are few things more distressing to a woman than watching her lovely locks fall out. More than two-thirds of women are affected by hair loss at some point in their life. Hair loss can range from thinning to bald patches. Yet, unlike men, women facing hair loss are offered few solutions to stop falling hair. There are three common, underlying causes of hair loss in women: low iron, hypothyroidism and nutritional deficiencies in the diet.
Low Iron and Hair Loss
Low iron is the main reason for hair loss in women and you do not have to be diagnosed with anemia to have your hair fall out. Your hair follicles contain ferritin which is your iron storage. When iron levels drop to low-normal, hair not only falls out, but it also becomes dry, breaks easily and loses pigment causing it to go grey prematurely. Severe hair loss can occur with low-normal ferritin.
Many women are diagnosed with alopecia when they actually have hair loss due to low iron. Have your ferritin and hemoglobin levels checked. A ferritin test result below 70 ug/L and hemoglobin below 140 ug/L will cause hair loss.
Studies show that we need 20 mg of iron daily from our diet, but most women are only getting 8 mg resulting in iron deficiency. Heavy menstrual bleeding should be addressed to ensure iron levels recover quickly.
Other common symptoms of low iron:
- No energy/fatigue
- Pale skin
- Breathlessness upon even minor exertion
- Dark under-eye circles
- Dizziness
- Thin, brittle or peeling nails
- Restless legs
- Cold hands and feet
Look for a micronized, microencapsulated iron pyrophosphate III supplement, which will increase iron levels quickly. Micronized, microencapsulated iron does not constipate or cause digestive upset like other iron supplements and it raises ferritin levels quickly.
Low Thyroid and Hair Loss
The second most common cause of hair loss is low thyroid, also called hypothyroidism. Have a thyroid stimulating hormone (TSH) blood test performed. Those with a TSH over 2.0 IU/mL will develop hair loss among other low thyroid symptoms. Your doctor will advise that thyroid is normal unless the TSH is over 5.5 IU/mL so ask for a copy of your test results.
If you cannot get thyroid hormone from your doctor and your TSH is above 2.0 IU/mL, take ashwagandha, gugguls, potassium iodide, tyrosine and selenomethionine to ensure that your TSH stays in the healthy range below 2.0 IU/mL.
Other common symptoms of low thyroid:
- Constipation
- Dry skin
- Weight gain or difficulty losing weight
- Sensitivity to cold
- Menstrual problems/heavy periods
- Fatigue or lethargy
Nutrient Deficiencies and Hair Loss
Lastly, a lack of protein or micronutrients (vitamins and minerals) in the diet can cause poor hair quality and hair loss. Eat protein at every meal along with a multivitamin with mineral supplement. If you are a vegetarian, vegan, or your diet is lacking, include a high quality, hormone-free, soy-free protein powder. Some good options are protein isolate, and pea, pumpkin, or hemp protein powders. Additionally, try taking 10 drops of choline-stabilized orthosilicic acid for thick, fast growing hair.
Quick Steps to Halting Hair Loss
- Have ferritin levels tested; if ferritin is below 70 ug/L, supplement with a micronized, microencapsulated iron pyrophosphate III supplement
- Have thyroid tested, TSH should be 2.0 IU/mL or below; if TSH is above 2.0 IU/mL, supplement with ashwagandha, gugguls, potassium iodide, tyrosine and selenomethionine
- Ensure you are getting enough protein in the diet by adding in a high-quality protein powder and eat lots of green vegetables
- Take a complete multivitamin and mineral supplement
- Supplement with choline-stabilized orthosilicic acid

Orgasm does not have to happen every time you make love, but it is a nice conclusion. If you do not have a partner, or you have not been able to have an orgasm with your partner, loving yourself is a sexually satisfying option for achieving an orgasm. It is also a great way to teach your partner what you need to reach orgasm. The key to the best possible orgasm is to be honest, and open with your partner about what you like and don’t like and what you need to feel great, whether it be a certain type of touch, kissing, or caressing.
Shed the Shame
The ‘M word’ has long been surrounded with taboos. Many illnesses have been attributed to masturbation—everything from hairy palms to blindness. Infants and children touch their genitals because it is pleasurable and makes them feel good. Depending on what you were told as a child by your parents to curb this behavior, you may think that masturbation is either a healthy, normal practice or a “dirty” one. Some people believe that masturbation should be censured because it stops people from seeking out another for sexual intimacy. Others believe if we promote masturbation, people will stop seeking out dangerous encounters that could lead to diseases like HIV, syphilis, or gonorrhea. Whatever your opinion of masturbation, let us start off by saying masturbation is not only normal, but also healthy. Women and men equally enjoy masturbation.
According to Lou Paget in her book The Big O, Orgasms: How to Have Them, Give Them, and Keep Them Coming, almost 70 percent of women cannot reach orgasm through penetration alone. There is nothing wrong with you if you are in this group; this is quite normal. Manual stimulation of the clitoris is required by most women. Paget also says that, for most women, the reason for no or few orgasms with a partner boil down to two issues: one, she isn’t being stimulated in a way that works for her; or two, she is not mentally present. As a result, it is often easier for a woman to be orgasmic on her own.
Self-Pleasure Steps
Put on some nice music, have a bath with your favorite aromatherapy products, light a candle, lock your bedroom door, put your lubricant on the bedside table, and relax. Don’t forget to breathe. Breathing is one of the most important aspects of great orgasms.
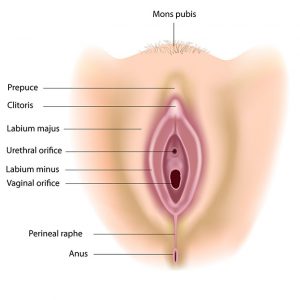
Touch your genitals—they are a pleasure center like no other. Try stroking or massaging all the areas of your genitals to find out how it feels. Some women like to use two fingers together. They begin stroking or rubbing on the upper part of the hood of the clitoris. Apply pressure to the mons pubis, massage your nipples, and caress the inner areas of your thighs. Explore the inner third of your vagina. Contract your vaginal muscles, and release, contract, and release. Experiment with different pressures and movements. Breathe in and out in a rhythmic manner. Get in tune with how your genitals feel. Women are often disconnected from this area of their bodies. It is time to reconnect.
Fantasize. Dream up images that make you feel sexy. Remember: no negative self-talk. If all of a sudden you find you are chastising yourself for having these thoughts, remind yourself that you are a beautiful, healthy, sexy woman who deserves to have great orgasms. There are no ‘dirty’ thoughts.
Self-stimulation is great if you are single or simply alone because it keeps your muscles working. Pelvic floor muscles get quite a workout during orgasm. The rhythmic contractions of orgasm give the walls of your vagina a workout too. Plus, orgasm can help those who have reduced lubrication by getting the secreting glands to keep working.
Masturbation helps relieve sexual tension when you are without a partner. No partner, no worries; masturbation to the rescue. For women who have partners with erectile problems, masturbation is a release and can take the pressure off his performance. And if you have yet to tell your partner how to satisfy you, then self-stimulation on your own is effective.
This experience is not about achieving orgasm. It is about getting to know what makes you feel great. If you reach orgasm, that’s wonderful. Betty Dodson, a famous sexologist, has written an excellent book called Sex for One, designed to teach self-stimulation. Every woman should get this book as a graduation present to help her understand her body and feel good about her genitals. Sex for One is not about eliminating your partner from the equation; it is about getting to know yourself. If you are with a partner, this will only enhance your relationship and open the door to some hot lovemaking. Masturbation is fun and will put you in touch with your body and connect your body to your mind.
Vibrators and Self Love
Sex toys, such as vibrators, can be a great way for women to increase their pleasure and learn what they respond to. In addition to being used alone, they can be used during intercourse or foreplay with a partner. Many women who have never had an orgasm found that they are able to achieve orgasm easier during intercourse after learning how to climax with a vibrator.
A Quick How-To
If you are new to using a vibrator, start by putting it on low speed. Buy a vibrator with a range of speeds, from low to intense. Start on low and place the vibrator on the mons pubis. Move it around until you find an area that feels sensitive and responsive, and alternate speeds. Some women place the vibrator just above the clitoris or the prepuce. If you put it on your clitoris, it can be over-stimulating and then you may not be able to have an orgasm. Many women who try a vibrator for the first time are shocked that they can have an orgasm in minutes. Lubricants can be used with toys.
Make sure to follow the clean and care instructions that come with each product. New toys should be cleaned before use and after each use. Regular inspections for damage are also important. Little cracks in the material are a breeding ground for harmful bacteria.
While the number of Canadians being diagnosed and dying of heart disease is decreasing, heart disease is still the second leading cause of death in Canada and the number one cause of death worldwide. Twenty-nine percent of Canadian deaths per year are due to a preventable condition that we can avoid by making heart-healthy choices.
Heart and Arteries: Friends for Life
The abundance of terms related to heart disease can get confusing. Heart disease is not just one condition. Many cardiovascular problems affect not only the heart’s ability to function well but also the blood vessels running throughout the body, which is why we often see cardiovascular issues in the brain, lungs and lower extremities, too.
Cardiovascular disease is an umbrella term for heart disease (including valve and rhythm issues), heart failure, diseases of the blood vessels and stroke. Coronary artery disease is by far the most common type of cardiovascular disease. Coronary artery disease is technically a disease of the arteries, the passageways that deliver—and restrict, if blocked—blood to the needy heart muscle. This disease often results in chest pain (angina) and heart attack. Another term you will often hear in this context is ischemic heart disease, which involves insufficient blood and oxygen flow to the body’s tissues.
Our Powerful Pump
Clench your fist, and there you have the approximate shape and size of your heart muscle nestled in behind your breastbone. The heart has four chambers—two upper (atria) and two lower (ventricles). Oxygen-depleted, bluish blood that has returned through the body collects in the right atrium, then flows down into the right ventricle. From there, it is pumped via the pulmonary artery to the lungs, where it picks up fresh oxygen. The now re-oxygenated, bright-red blood travels through the pulmonary veins back into the heart, but this time, it flows into the left atrium and then down into the left ventricle. Finally, it leaves the heart through the aorta to begin its next cycle throughout the body.
The heart beats an average of 100,000 times a day. Day in, and day out, from birth to death (upward of 2.5 billion heartbeats), it delivers oxygen, nutrients, hormones and other essential constituents to every cell in our body. At the same time, the blood collects cellular junk—the unwanted waste of regular processes that occur inside cells. Think of this mighty heart muscle as the pump that keeps everything else running. Just like a mechanical pump needs fuel to keep working, the heart requires a steady supply of blood and oxygen to stay healthy. Problems arise when it does not get this fuel because somewhere in the system, a blockage has occurred.
Our Artery Helpers
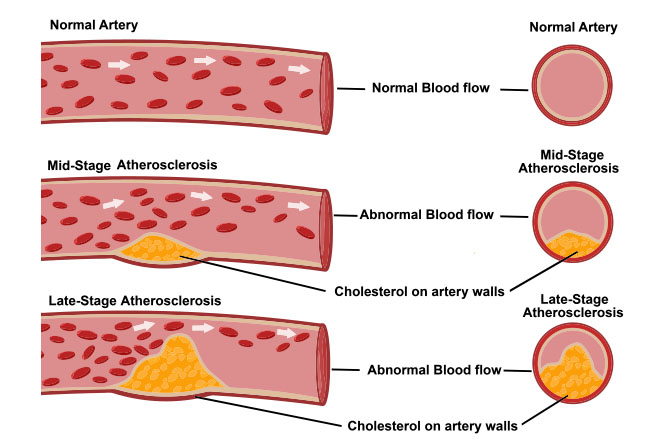
The heart has two major arteries: the right coronary artery and the left main coronary artery. Each of these arteries stretches out into smaller and smaller arteries, delivering blood deeper into the heart muscle cells. If the blockage develops in one of these arteries, we call it atherosclerosis from the Greek athere, meaning “porridge,” and sclerosis, meaning “hardening” or “scarring.” Over time, plaque builds on the arterial walls and causes them to stiffen. This accumulation narrows the arteries, and blood clots sometimes form on top of the plaque. The result is reduced blood flow through the heart. A heart attack (or myocardial infarction, meaning “death of heart tissue”) occurs if blood flow stops completely.
The most common reason for reduced blood flow to the heart is atherosclerosis. However, there are other possible reasons for blocked arteries. Blood could be too thick, for instance. Ideally, blood is thin so it can pass unheeded through increasingly tiny passageways on its way to and from cells. Sometimes, red blood cells must bend and squeeze through a single file because the arterial tunnel is so tiny! Blood thickens, and the cells clump together if the body’s clotting factors are affected. Our poor circulation then slows, and the heart is forced to work harder to counteract the effects of fatty blood.
Sometimes, the reason behind diminished blood flow lies with the heart muscle itself. Maybe it has been weakened or damaged from a previous heart attack. Or the left ventricle, which pumps freshly oxygenated blood back into the body, has been damaged by high blood pressure. The left ventricle is particularly relevant to heart disease. Uncontrolled high blood pressure can cause poor left ventricle function and worsen heart disease.
Arteriosclerosis vs. Atherosclerosis
What is the difference between arteriosclerosis and atherosclerosis? They both relate to arteries, but arteriosclerosis is any process that causes damage and hardening or thickening of our major arteries. Atherosclerosis is the most common form of arteriosclerosis and explicitly involves the nasty buildup of artery-toughening plaque. When plaque buildup happens in the coronary arteries, we get heart disease. When it happens in other parts of the body, we get impaired circulation, which can cause strokes, blood clots, and leg problems involving poor circulation, ulcers, poor wound healing, and gangrene.
Clogged Pipes
Far from being an inanimate pipe, our arteries are a player in this inner game of life. They contract and expand in response to pressure.
Arteries have three layers, the outer, tougher adventitia; the middle smooth muscle media; and an inner layer (intima) lined with a single layer of specialized cells called the endothelium. This last ultra-thin barrier is a crucial component in the development of atherosclerosis. Besides their ability to gauge blood pressure and flow, these multi-functioning endothelial cells interact with substances carried by blood, produce compounds that affect cell growth, and help govern muscle tone, thus allowing arteries to expand and contract. This expansion and contraction of arteries push blood to where it is needed.
Unfortunately, the endothelium layer frequently gets injured. The possible causes are many, including physical force and high blood pressure. Blood also carries toxins (environmental, dietary, metabolic), fatty proteins, excess blood sugar (glucose), infectious microbes and unhealthy cholesterol. These can cause endothelial dysfunction and trigger events leading to atherosclerosis, high blood pressure, heart attack, stroke, and heart failure.
The Role of Cholesterol
Cholesterol has gotten a bad rap. Our bodies produce cholesterol—a waxy, fatty substance—which performs several important functions. Cholesterol is the building block of cellular membranes and is needed to make bile acids so we can digest and absorb our food. It is also necessary to make vitamin D and hormones. To move through the bloodstream, cholesterol puts on a protective coat of lipoprotein particles: low-density lipoprotein (LDL), the “bad” cholesterol, and high-density lipoprotein (HDL), the “good” cholesterol. Generally, we want to keep LDL cholesterol levels down to prevent it from lodging in arterial walls. Conversely, we want higher HDL cholesterol levels, which protects the heart by sweeping LDL cholesterol through the arteries towards the liver. Here it is processed, then excreted from our system.
When endothelial cells are damaged, they trigger an immune response. The body sends in a repair team to address the inflamed injury, but other scroungers also show up: blood fats and bad LDL cholesterol. Now, rather than help with repairs, immune cells begin an overzealous inflammatory process. As they migrate into the artery wall to help the injury, they ingest the LDL cholesterol and form bloated, fatty foam cells that form atherosclerosis plaque. The damage is worse if the LDL cholesterol is oxidized, i.e., previously damaged by free radicals. Oxidized LDL cholesterol also damages neighboring cells at the injury site in a chain-reaction-type effect.
Free Radicals and Antioxidants
Think of rust for a minute. Slowly, various chemical reactions occur resulting in an invasive corrosion that is the bane of every vehicle owner’s existence! The damage created by free radicals in the body is like rust.
Free radicals are a natural byproduct of everyday reactions that produce energy for the body. Other major sources and generators include:
- Eating fried foods, oils heated over their smoking point, and rancid fats
- Eating nitrates and nitrites in meats
- Toxic airborne chemicals
- Cigarette smoke, or smoke from forest fires
- Exposure to medical or electromagnetic radiation (i.e., computer terminals)
- Excessively strenuous exercise
- Drinking chlorinated water
- Eating a high-fat diet
- Eating processed foods
- A diet high in sugar
- Prolonged physical and/or emotional stress
Many free radicals are highly toxic, mutagenic (cause cells to mutate), and carcinogenic (cause cancer). What these tiny molecules lack in size, they make up in destructive capacity. Stable molecules are held together by two electrons, but free radicals are missing one electron they attempt to steal from neighboring molecules. Such molecular theft causes an undesirable ripple effect where other molecules in cells and cell membranes are damaged, and more free radicals are formed. Eventually, if left unattended, what was once comparable to a spot of rust becomes a car riddled with unsightly holes.
Antioxidants are free radical scavengers. They readily disable free radicals, preventing healthy body tissues from being damaged. When the body is deficient in antioxidants, our risk of disease increases, and aging accelerates. The progression of free radical damage can, fortunately, be kept in check with antioxidants from our food and nutritional supplements.
By eating foods rich in antioxidants such as vitamins A, C, and E, selenium and phytochemicals (the pigments that give plants their colors), we can keep our defences against free radicals strong and stave off their heart-unfriendly effects. Supplemental pycnogenol, sytrinol and coenzyme Q10 serve the same important function, and further protect against heart disease.
When Plaque Ruptures
As atherosclerosis progresses, the arterial plaque grows and hardens as more cholesterol is absorbed into the artery wall, other fats, and inflammatory cells. A cap form over this. Some are big; some are small. Smaller plaques are more dangerous because they have a greater tendency to rupture in response to a variety of physical and emotional triggers. When this plaque ruptures, the immune system erroneously orders the production of factors that dissolve the plaque cap, causing its contents to spill back into the artery. Another immune response kicks in, attracting blood platelets. They clump together around the ruptured plaque and, along with red blood cells and other clotting factors, form a blood clot. A heart attack results if that blood clot entirely blocks a coronary artery.
How tragic that the first symptom of heart disease to be taken seriously is usually a heart attack and, sometimes, death.
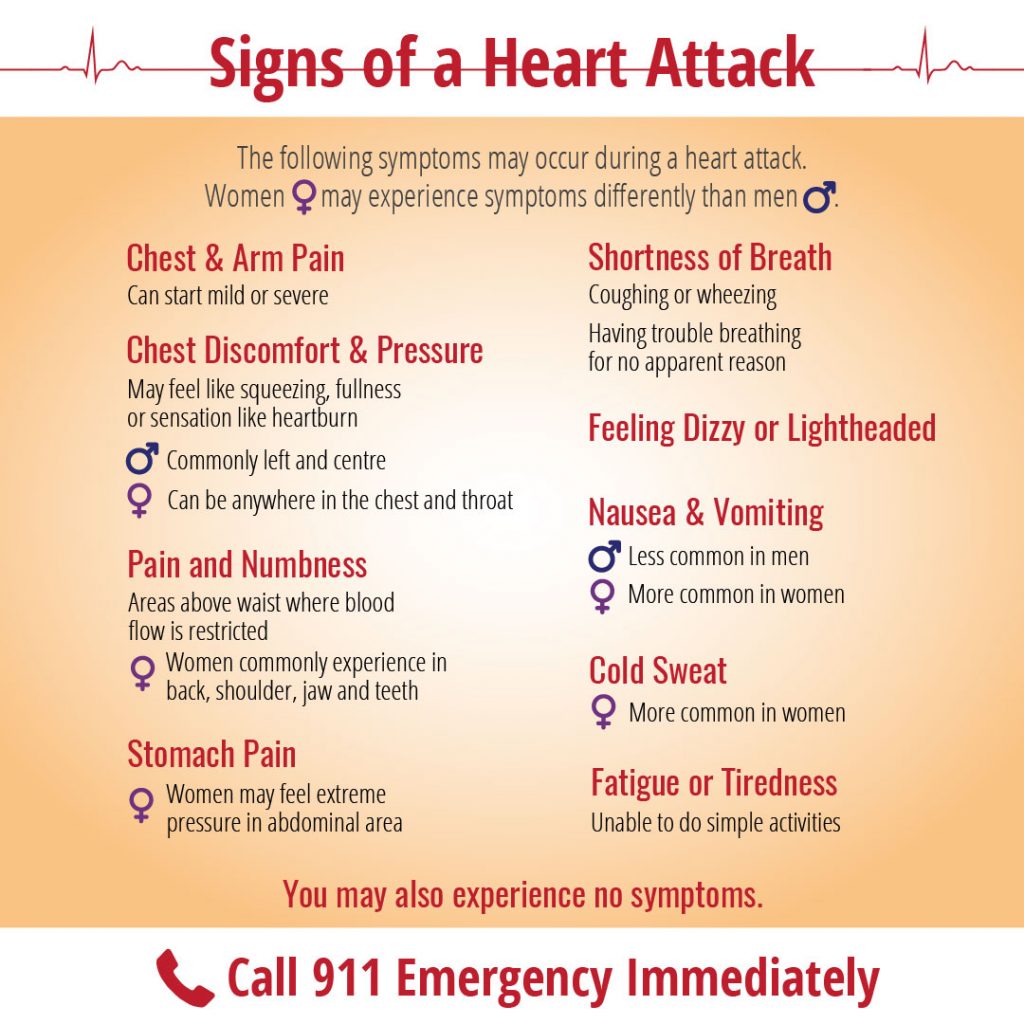
The problem often lies in our general disconnect from our bodies. We are under such stressors in daily life that we miss or disregard many warning signs like chest pain, which occurs when coronary arteries narrow by about 50 percent. Medically termed angina (Latin for “squeezing of the chest”), symptoms include:
- Pain radiating from the chest that spreads to your left arm, neck, back, throat or jaw
- Tightness, pressure, squeezing and/or aching in your chest or arm(s)
- Persistent sensation of moderate to severe indigestion
- Sharp, burning or cramping pain
- An ache starting in, or spreading to, your neck, jaw, throat, shoulder, back or arm(s)
- Neck or upper back discomfort, particularly between the shoulder blades
- Numbness in your arms, shoulders or wrists
Women with angina are more likely to notice abdomen, shoulder and back discomfort than men. Likewise, with actual heart attacks, symptoms vary between the sexes.
In the case of a heart attack or symptoms leading up to it, the quicker medical attention is sought, the greater the chances of avoiding heart damage. The longer the blood supply is impeded or cut off, the more damage the heart potentially sustains. After 20 to 40 minutes, damage can be irreversible. Living tissue becomes scar tissue.
When women get a diagnosis and treatment, it usually occurs when they are older, and heart disease is more advanced. Sadly, women are more likely to brush off bouts of warning signs, perhaps fearing embarrassment. Women are also more likely than men to drop out of cardiac rehabilitation programs after a heart attack.
Other Heart Conditions
Arrhythmias
Usually, the heart beats 60 to 100 times per minute with the same lapse between each beat. Arrhythmia represents an irregular rhythm. There are several types of arrhythmias which vary in degrees of risk. Some are linked to underlying heart disease, others to low thyroid, iron deficiency, anemia, magnesium deficiency, and stress.
Ventricular tachycardia and ventricular fibrillation are potentially fatal. In atrial fibrillation, which occurs in one percent of people over the age of 60, the heart seems to quiver instead of beating regularly because electrical impulses have been disturbed. If the underlying cause is treated, an arrhythmia will often settle down on its own.
Valve Disorders
With mitral stenosis, the heart’s mitral valve has a narrowed opening that restricts blood flow from the left atrium into the left ventricle. Shortness of breath results when blood pressure builds up in the atrium and affects the lungs. If the valve develops a leak, blood flows backward into the heart chamber, requiring the heart to work harder and, over time, possibly resulting in heart failure. Causes include mitral valve prolapse, infectious bacteria or a damaged heart muscle.
In aortic stenosis, a narrowed aortic valve reduces blood flow from the heart to the rest of the body. The left ventricle enlarges due to the strain, possibly resulting in angina or faintness. If left unrepaired by surgery, congestive heart failure and death may result. The aortic valve can also develop a leak, eventually causing heart failure if untended.
Heart Failure
When the heart muscle is weak, damaged and/or abnormally thick, it becomes an inefficient pump. The result is insufficient blood flow to the body that leads to heart failure. As the body tries to compensate, symptoms include a higher heart rate, increased blood pressure and fluid retention. As the current population living with heart disease rises, so does the incidence of heart failure. Acute heart failure occurs when the heart suddenly stops pumping efficiently. Blood backs up in the pulmonary veins, and the pressure causes the lungs to fill with fluid (pulmonary edema), creating an emergency situation.
The most common cause of heart failure is coronary artery disease, which usually occurs after one or more heart attacks and resultant high blood pressure. Other causes include valvular heart disease, inflammatory viruses and diseases, and damage caused by alcohol and drug use. Symptoms include swelling (edema) of the legs, feet or abdomen, shortness of breath, a nighttime cough, fatigue, chest pain and pressure, weight gain and dizziness. Keep in mind that not everyone with progressive heart failure exhibits symptoms.
Interestingly, we now know that heart failure differs between the sexes. In men, it is usually due to systolic dysfunction, meaning that the heart is weakened, enlarged and cannot sufficiently pump blood throughout the body. This is often referred to as a “floppy heart”. Women, meanwhile, have what is described as a “stiff heart” that is associated with what is known as diastolic dysfunction, meaning that the heart’s ability to relax between beats is impaired. A stiff heart muscle is small and cannot fill normally with blood. Regardless of whether your heart is floppy or stiff, heart failure is treatable and should be monitored.
Prevention is Best
The expression “Prevention is a pound of cure” applies to no condition better than to heart disease. By taking proactive steps to address those risk factors we can change, we can stave off or even avoid intrusive conventional medical treatment and reduce the need for medications. A multidimensional approach to heart health greatly improves our quality of life, and helps return our focus to the things that matter most in our lives.
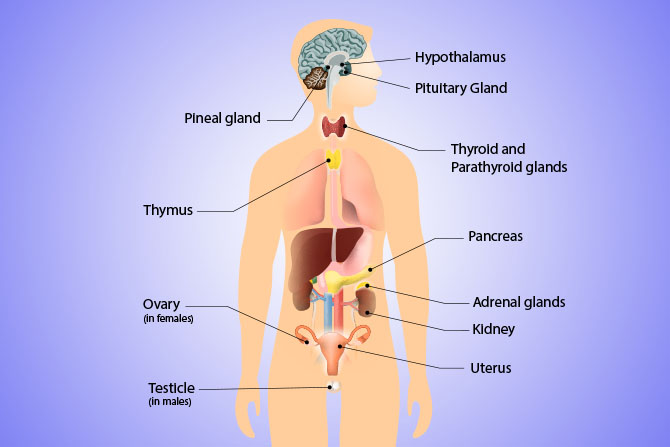
The endocrine system is made up of glands that produce hormones. Hormones are chemical messengers that tell other systems throughout your body what to do, how to do it, and when to do it. The messages they send could be to make you sleepy like melatonin does; or to rev up your energy supply to meet the next deadline, which is what occurs when cortisol is secreted; or raise your blood pressure, which aldosterone can do; or to release an egg, like luteinizing hormone signals, or get you in the mood for love (thanks to an increase in testosterone).
Many hormones are secreted in the body—over 50 are known at the moment. There are thousands of body processes that occur because of your hormones. This “complicated” interaction means that if you tinker with one component of a hormone process, you may interfere with every process related to it. There can be a domino effect (or a “cascade effect”) that can affect every hormone down the chain.
Remember this: hormones work together. When the correct amount of the right hormone is in the right place at the right time, you have beautiful, clear skin; strong bones; and a great sex drive. You have strength and stamina, are breast-cancer-free, and prior to menopause, you are fertile (as Nature intended you to be).
Hormone Messengers Control the Body
You were not born with a lifetime supply of hormones. Organs, glands, and cells in your body, mostly those in your endocrine system, secrete hormones into your bloodstream. Once it has traveled through the bloodstream, the hormone acts like a key that fits into a lock on specific target cell membranes. The lock is called the receptor. Sometimes the hormone (the key) fits the lock exactly, and other times it alters the action of the lock. Some of these “locks” can take more than one key (meaning several hormones can affect it).
The endocrine system makes these powerful messengers day in and day out from building blocks like cholesterol, amino acids found in protein, or components of fats in your diet. The three types of hormones are summarized in the table below.
| Hormone Type | Source(s) | Selected Examples |
|---|---|---|
| Steroid hormones |
|
progesterone, testosterone, estrogens (including estradiol, estrone, estriol), cortisol, prostaglandins, DHEA (dehydroepiandrosterone) |
| Peptide (protein) hormones |
|
insulin, luteinizing hormone, follicle-stimulating hormone, prolactin, growth hormone, dopamine, antidiuretic hormone |
| Amine-derived hormones |
|
melatonin, serotonin, epinephrine, thyroxine |
In the presence of stressors, the immune system and endocrine system work as an integrated circuit. Deficiencies in the immune system and abnormalities in the cross talk with the endocrine system can make a person more susceptible to developing chronic inflammatory disease, autoimmune disease like lupus, rheumatoid arthritis, a reduced ability to fight infections, osteoporosis, muscle atrophy, rapid aging, poor antibody production against vaccines, and more. Modulating or keeping cortisol levels in balance through a healthy diet, nutritional supplements, and stress reduction are key to disease prevention.
Hypothalamus
The hypothalamus sits just below what is called the base of the forebrain, so it is in the lower part of the front of the brain. It manages the regulation of the body’s internal environment by taking signals from the nervous system and sending out hormone messages to the pituitary gland, directing it to either start or stop a hormone process.
The Pituitary Gland
The pituitary gland is only about the size of a pea, but it has a front and a back— the anterior lobe and the posterior lobe—that each produce specific hormones in response to a signal from the hypothalamus. The instructions for action that go out to the kidneys, uterus, mammary glands, thyroid, adrenal cortex, ovaries, and bones and tissues come from the pituitary gland.
Adrenal Glands
The two adrenal glands are among the most important glands in the body. These small glands release the stress-response hormones that guide the body’s reaction to a stressor, as well as small amounts of estrogen, testosterone, DHEA, cortisol and progesterone. The accumulated effects of internal and external stressors have a profound impact on the adrenal glands, an impact that ripples out into the area of hormone health.
Each adrenal gland sits on top of one of the kidneys and contains two parts: the adrenal medulla and the adrenal cortex. In response to triggers from the hypothalamus, the adrenal medulla secretes hormones called epinephrine (aka adrenaline) and norepinephrine. These hormones are part of the “fight-or-flight” response that cause that fast, short-term increase in blood sugar levels; breathing rate; cardiac output; blood flow to the muscles, lungs, and brain; and cellular metabolism that can get you moving when you think you are in danger.
The adrenal cortex is responsible for the production of a wide range of hormones called glucocorticoids, including cortisol, and the mineral corticoids aldosterone and testosterone. This release happens in response to a signal from the pituitary gland and results in a longer-term stress response that increases blood glucose as well as suppresses your immune response, in order to concentrate your energy on dealing with the stressor.
The secretion of hormones by the adrenal cortex in response to stress is one of the most important functions of the adrenals as these hormones help you adapt to the stresses of life over the longer term. Various adrenal hormones stimulate the conversion of protein to energy, so that energy levels remain high even after the glucose released for the fight-or-flight reaction has been used up. The adrenal hormones help maintain elevated blood pressure and create changes needed for dealing with such stressors as emotional shocks, infection, high workload, weather changes, environmental chemicals, or physical or emotional trauma.
Over time, particularly a period of continual exposure to stressors, it is possible for the adrenal glands to become exhausted and unable to secrete the necessary hormones. Adrenal exhaustion is a serious concern because the adrenal glands secrete both male and female sex hormones—estrogens and androgens—and become the prime producers of estrogens and progesterone when the ovaries “retire.”
In today’s world, most women (and people in general) have some degree of adrenal compromise. Women are generally working a full-time job, raising children, and juggling hundreds of other demands of daily life. Poor adrenal health undermines a woman’s ability to make the transitions inherent in female life smoothly. In particular, it can compromise sleep quality, which in turn further compromises adrenal function.
Many medical doctors do not recognize adrenal exhaustion unless the glands become so compromised that disorders such as Addison’s disease or Cushing’s syndrome occur. Until adrenal exhaustion is recognized, the person will most likely have suffered for years from symptoms of under- or overactive adrenal function. Years of chronic stress eventually cause poor adrenal function, but prior to the organ becoming compromised, there are usually periods of over-activity that, if untreated, usually result in inadequate adrenal function.
Some people, however, stay in the overactive state for a prolonged period. Menopausal symptoms resemble those of Cushing’s syndrome, a disease related to over-activity of the adrenal cortex. For example, hot flashes, night sweats, and insomnia, which are common menopausal symptoms, are also symptoms of Cushing’s syndrome, which is caused by chronic exposure to excess levels of cortisol.
Thyroid Gland
The thyroid gland, located at the front of your throat, sets the rate of your body’s metabolism, which means it regulates nearly every cell in your body. This butterfly-shaped gland receives messages from thyroid-stimulating hormone (TSH) from the pituitary and secretes thyroxine (T4) and triiodothyronine (T3), which travel through your bloodstream and affect the rate that your body metabolizes fats, proteins, and carbohydrates for energy at many sites. In other words, thyroid hormones set the rate for the way you use food as fuel, rev up your fat-burning furnace, and set your heart rate and temperature, among dozens of other important functions in the body.
Calcitonin, another hormone secreted by the thyroid, is involved in the balance of blood calcium levels. It lowers the amount of calcium and phosphate in the blood as necessary by inhibiting bone breakdown and accelerating the assimilation of calcium. Calcitonin stimulates movement of calcium into bone in opposition to the effects of parathyroid hormone (discussed below). Any change in thyroid function has far-reaching effects, including slowing down your fat-burning furnace, which causes you to gain weight; affecting your heart rate and your fertility; and promoting bone loss.
Because thyroid hormones regulate every cell—in every organ—keeping your thyroid healthy and your levels of thyroid hormones balanced is another key to vibrant health.
The Thyroid and Adrenal Connection
The thyroid—adrenal feedback interaction is orchestrated by the nervous system. Stressors on the body and the resulting chronic secretion of cortisol from the adrenal glands have a negative impact on the thyroid gland. When cortisol goes up, estrogens increase. Estrogens block the uptake of thyroid hormone. So stress on your adrenals has a negative effect on the thyroid, causing reduced uptake by thyroid hormone receptors and low thyroid hormone output. Adequate amounts of thyroid hormone are needed to make cortisol function properly and vice versa. So interdependent are these two hormones that they share many of the same deficiency or excess symptoms when they are not in balance.
When the adrenal glands are overworked due to stress, working too much, not enough sleep, or poor diet, the body converts progesterone into adrenal hormones, which depletes your body of progesterone. Thyroid hormones and progesterone feed information back to the pituitary, helping to balance other hormones and thereby help the adrenals—which, like the thyroid, are stimulated by the pituitary—with stress adaptation. When progesterone levels are low because of its conversion into stress-fighting hormones, the thyroid suddenly has to take on the task of sending hormones to the pituitary with little outside help.
As we noted, the thyroid determines your metabolic rate. If your adrenals are depleted, your thyroid will force them to maintain the proper rate. However, this type of pressure on your endocrine system over time leads your thyroid to decrease hormone production in order to conserve energy. When this first happens, symptoms of low levels of both adrenal and thyroid hormones occur. If the symptoms are not addressed, over time they will come to be predominantly related to one gland or the other— usually your thyroid.
The Thyroid and Liver Connection
Some non-endocrine organs, such as the heart, lungs, liver, large intestine, and skin, also play a regular part in maintaining optimal levels of key hormones. A healthy liver is particularly important if you hope to avoid hormone havoc. Your liver can break down and eliminate excess hormones to help maintain the correct levels. It also manufactures the cholesterol that is used to make the key sex hormones including testosterone, estrogen, progesterone, and DHEA.
The thyroid is influenced by the function of the liver. The liver governs the flow of fluids through the body. When the liver is congested or stagnant, swelling (edema) occurs. This congestion may occur in the thyroid area. When a noticeable enlargement of the thyroid occurs—called a goiter—this is also a sign of liver congestion.
Research indicates that thyroid problems are on the rise because of the widespread poor nutritional status of people today. Thyroid hormones are made from protein and minerals. Vitamin D made from sunshine on the skin is also a key nutrient for thyroid hormone manufacture. Vitamin D deficiency is common in the Northern Hemisphere. As well, the high levels of environmental toxins to which people are exposed affect liver function. The liver’s ability to eliminate toxic compounds and so support good thyroid functioning depends on the strength of its detoxification systems, which, in turn, are directly influenced by diet and lifestyle.
The Parathyroid Gland
The parathyroid gland is made up of four small glands that are adjacent to your thyroid. It secretes parathyroid hormone (PTH), the hormone that stimulates bone cells to break down bone and release the stored calcium whenever your body detects a low concentration of calcium in your blood. PTH is thought to be more important than calcitonin for bone health as those who have had their thyroid removed but still have healthy levels of PTH maintain normal calcium metabolism. PTH is also involved in the absorption of food by the intestines and the conservation of calcium by the kidneys.
Pancreas
Your pancreas is a gland that is about six inches long; it sits behind your stomach and is connected to your small intestine. It assists in the work of digestion by secreting digestive enzymes, but it also takes on an endocrine function by secreting the hormones insulin and glucagon directly into your bloodstream. These two hormones are a tag team: insulin’s job is to push glucose (sugar) into cells and decrease your blood level of glucose; glucagon increases the level of glucose in your blood when it gets too low. The pancreas monitors the levels of glucose in your bloodstream and secretes one of those two hormones to make the adjustments and keep your blood glucose levels where they should be. (When blood sugar levels are constantly too high, the pancreas can become exhausted from chronic insulin production, and this leads to the reliance on insulin drugs.)
Ovaries
When the pituitary gland sends out follicle-stimulating hormone and luteinizing hormone, the target organ is mainly the ovaries. The ovaries are the storage organ for the eggs, held inside the follicles. The average woman is born with over a million follicles, and each one contains an immature egg. By the time menstruation begins, many of these follicles have degenerated and a woman may have half as many eggs as she had at birth. Every month up to 20 follicles begin maturing. An increase in follicle-stimulating hormone (courtesy of the pituitary gland) stimulates the full maturing of one egg (or, less often, multiple eggs).
Luteinizing hormone (LH) is the hormone that stimulates the release of the egg from the ovary. Fallopian tubes on either side of the uterus, not attached to the ovary, act as portals for the egg to the uterus, sweeping up the egg that has been released and ensuring its passage to the uterus. Meanwhile, the LH stimulates the spent follicle (now known as a corpus luteum) to release progesterone and some estrogen.
The Ovary and Thyroid Connection
There is a direct relationship between the ovaries and the thyroid gland. Next to the thyroid, the ovaries contain the greatest concentration of iodine in the female body, so when iodine is deficient, you will feel the effects in both the ovaries and the thyroid. But most importantly, the ovary has hormone receptors for thyroid hormones. These receptors for thyroid hormones play a role in development of the egg and conception. Also, too much thyroid hormone activity may increase estrogen receptor function and too little thyroid hormone activity on the ovary can create menstrual problems and infertility.
Research in the Journal of Clinical Endocrinology and Metabolism in 2007 evaluated the ovarian surface epithelial cells for hormone receptors, including those for thyroid hormone. The ovaries from women who had had a hysterectomy were used. Researchers found that the ovarian surface is a target for T3 thyroid hormone and that T3 hormone increased the action of estrogen receptors. They believed this discovery could help explain the link between hyperthyroidism (too much thyroid hormone) and ovarian cancer. But if your levels of thyroid hormone are low, this could have huge implications for the level of estrogens, as well as the functioning of your reproductive system and your sex drive.
In 2000, a group of Slovakian doctors found clear evidence of the ovary/ thyroid connection when they used pure thyroid gland extracts to treat young, infertile women who had menstrual cycle dysfunction. By giving the infertile women pure thyroid hormones, doctors had improvement of the women’s menstrual cycles, which ultimately led to conception. In previous studies, the doctors had discovered the presence of thyroid-stimulating hormone and T3 receptors in the ovary. They found that T3 had a direct effect on egg maturation. With up to 30 percent of North American women walking around with undiagnosed low thyroid, many women could be suffering with ovarian issues and infertility that could be cleared up with thyroid support.
There is also a clear connection between polycystic ovary syndrome (PCOS) and autoimmune thyroiditis. According to the March 2004 European Journal of Endocrinology, women with PCOS were almost seven times more likely to have autoimmune thyroid disease than women without PCOS. Women with PCOS rarely form a corpus luteum (which releases progesterone), and therefore these women do not manufacture appropriate levels of progesterone. Endocrine researchers have shown that low progesterone levels lead to an overstimulation of the immune system in women with PCOS, causing autoimmune thyroiditis and other immune abnormalities predominantly found in women, including multiple sclerosis and lupus.
The ovaries are the organs that get the “bad rap” during menopause and in other hormone-related disorders. They do play an important role, but, as we’ve noted, the ovaries are only one player in the large hormone orchestra.
Pineal Gland
The cone-shaped pineal gland is located deep in the brain. Its function is not well understood, however it is known to make melatonin and secrete it into the bloodstream. Melatonin is the hormone that regulates the sleeping and waking cycle.
Hormone Factory Summary
| Endocrine Gland | Hormones Secreted | Key Functions/Effects |
|---|---|---|
| Hypothalamus | Stimulating and inhibiting hormones that turn processes on or off | Sends hormonal instructions to the pituitary gland |
| Pituitary | Human growth hormone (hGH)
Thyroid-stimulating hormone (TSH) Follicle-stimulating hormone (FSH) Luteinizing hormone (LH) Prolactin (PRL) Adrenocorticotropic hormone Antidiuretic hormone (ADH) Oxytocin (OCT) |
Sends out hormones that stimulate activity in other endocrine organs such as the thyroid (TSH), the ovaries (FSH, LH), the mammary glands (PRL, OCT), the adrenals (ACTH), the kidneys (ADH), as well as stimulating bone and muscle growth and metabolism (hGH) |
| Adrenal (cortex and medulla) | Aldosterone
Cortisol, epinephrine (adrenaline), norepinephrine DHEA |
Regulates sodium and water
Sustains the stress reaction by raising blood glucose levels and helping to break down protein Blood pressure and stress |
| Thyroid | Thyroxine (T4)
Triiodothyronine (T3) Calcitonin |
Helps regulate the rate of metabolism |
| Parathyroid | Parathyroid hormone (PTH) | Helps regulate bone status and blood calcium |
| Pancreas | Insulin
Glucagon |
Lowers blood glucose levels
Raises blood glucose levels |
| Ovaries | Estrogens | Promotes formation of female secondary sex characteristics
Stimulates endometrial growth Increases uterine growth Maintenance of vessel and skin Reduces bone resorption; Protein synthesis Coagulation; increases antithrombin and plasminogen; increases platelet adhesiveness Lipid function; increases HDL, triglyceride, fat deposition; decreases LDL Balances salt and water retention Gastrointestinal tract function; reduces bowel motility; increases cholesterol elimination |
| Ovaries | Progesterone | Assists in thyroid function, in bone-building by osteoblasts, in bone, teeth, gums, joint, tendon, ligament and skin resilience, and in some cases healing by regulating various types of collagen, and in nerve function and healing
Increases core temperature during ovulation Reduces spasm and relaxes smooth muscle Acts as an anti-inflammatory agent and regulates the immune response Reduces gall-bladder activity Normalizes blood clotting and vascular tone, zinc and copper levels, cell oxygen levels, and use of fat stores for energy Appears to prevent endometrial cancer (involving the uterine lining) by regulating the effects of estrogen |
| Pineal (located in the brain) | Melatonin | Helps control sleep/wake cycles, is an antioxidant, supports healthy immune function |
Your Fat Cells Are Also Hormone Factories
Fat cells (also called adipose tissue) are located in different places in men and women. Men tend to carry body fat in their chest and abdomen. Women carry it in their breasts, hips, buttocks, thighs, and waist. Estrogen and testosterone play a role in the deposit of fat on the body. And there are two types of fat: white fat and brown fat. White fat insulates you from the cold, cushions your structure, and is used as fuel for energy. Brown fat is very important for producing heat (thermogenesis). Brown fat cells contain mitochondria, the energy producers of the body, which is why they can generate heat.
There are also two types of obesity: one in which fat cells are too large (called hypertrophic obesity) and another in which the person has too many fat cells (called hyperplastic obesity). The size of fat cells can change throughout life, but the number of fat cells is determined by the late teens. Having too many fat cells is a product of the types of foods your mother consumed while she was pregnant and/or if she developed gestational diabetes, as well as the amount of food fed to you throughout your childhood. (Remember this if you are going to have children or have babies or toddlers.) During the third trimester of fetal development, and then later at the onset of puberty, fat cells are formed at increased rates. This is why healthy, appropriate prenatal and teen nutrition play a role in weight management as an adult.
From a hormone perspective, the size and number of fat cells also affect adult hormone balance. Scientists around the world have found that fat cells, swollen to capacity with stored fat, spew out vast amounts of hormones and chemical messengers that hasten death from heart disease, strokes, diabetes, and cancer. Fat cells are hormone factories, using androstenedione and the enzyme aromatase to make estrogens. These estrogens in the system are in addition to those produced elsewhere and can be a source of estrogen-dominant conditions.
Moderately obese people cut their lifespan by up to five years, and the severely obese see a reduction of at least ten years. Fat cells are now viewed as one of the most important endocrine cells in the body. Fat cells secrete approximately 25 signalling compounds—including estrogens, resistin, leptin, adiponectin, inflammatory proteins, tumor necrosis factor-alpha, interleukin-6, growth hormone, and more—that are sending out messages that can promote or weaken dozens of deadly health conditions and negatively affect your sexy hormones.
How else can fat cells harm your health?
Doctors used to think that high blood pressure associated with weight gain simply occurred because the person had to push blood through more mass. Now, with the discovery that fat cells can manufacture a potent constrictor of blood vessels called angiotensinogen, researchers know that action of this chemical is a major contributor to high blood pressure in the over-weight—and why the fat cells are killing them. Combine this blood-constricting hormone with the inflammatory factors produced by the fat cell, and artery walls develop a build-up of tissue that blocks blood flow, thus increasing the risk of stroke and heart attack.
The growth hormone and estrogens produced by fat cells also fuel cancer cells. Obese women are at much higher risk of developing estrogen-dominant cancers, particularly breast cancer, and they are more likely to die from the disease because their fat cells pump out copious amounts of estrogens. Overweight women who have not gone through menopause have an increased risk of developing polycystic ovary syndrome, ovarian cysts, fibrocystic breasts, migraine headaches, uterine fibroids, endometriosis and acne as a result of their bulging fat cells.
Those xenoestrogens (estrogen mimickers absorbed from environmental plastics, cosmetics, hair dyes, pesticides, PCBs, parabens, glycols, and hundreds of other chemicals) discussed earlier are stored in fat cells. Even an extra 10 pounds (4.5 kg) of fat increases these deadly estrogens that disrupt hormone balance in the body, congest the liver, and further increase rates of cancer.
The fat cell can be thought of as an active manufacturing facility of hormones with lots of fat-storage capacity that can maintain its size.
Fat Cells and the Liver
Any disruption of the liver detoxification pathway contributes to excesses or imbalances in hormones and toxins and fat gain. The liver is also responsible for conjugating (combining) estrogens and other steroid hormones, certain drugs, and chemical compounds. Too much estrogen is one reason why women have a difficult time losing fat around the abdominal area. A decreased rate of estrogen excretion because of poor liver detoxification contributes to what we commonly call “estrogen belly,” which is simply too much fat around the middle, promoted by having too much estrogen due to faulty excretion of excess estrogens.
Too much fat on your body also increases your estrogen levels. This is because fat cells are not only involved in manufacturing estrogen via the enzyme aroma-tase but are also a storage site for estrogen. This sets up a vicious cycle of too many fat cells manufacturing and storing too much estrogen, which creates high levels of estrogen, which maintains increased fat and larger fat cells and causes hormone disruption.
Fat Cells and Insulin
Insulin, a hormone secreted by the pancreas, is another culprit contributing to “fatness.” The standard, excessively high-carbohydrate, low-protein diet disrupts the body’s ability to regulate blood sugar adequately. When too much insulin is being pumped out to reduce abnormally high blood sugar (by storing it in fat cells), the body inevitably gains weight, becomes fat, and cells become very resistant to insulin (leaving glucose in the bloodstream) and fat loss. Everyone who is overweight is at risk of insulin resistance, and insulin resistance puts them at higher risk of heart disease, cancers, diabetes, polycystic ovary syndrome, facial hair growth, anxiety, and more.
Endocrine Summary
As you can see, the key organs of the endocrine system do not work alone. Just as hormones work together, so do the organs that produce them. The relationships among them, particularly related to the thyroid, ensure that you are feeling fabulous when a partnership is working and not well at all when a pair is out of tune.
The amount of hormone secreted by the glands and organs of the endocrine system is determined by the body’s need for the hormone at any given time. It is important to understand, especially when we start discussing hormone therapies, that a single hormone can promote a cascade of events in the body. For example, one of the side effects of high-dose oral estrogen therapy or exposure to high levels of environmental estrogens is low thyroid function because estrogen blocks the uptake of thyroid hormone. Through complex feedback mechanisms, hormone production is regulated so that there is no over- or underproduction of particular hormones. When women start adding hormones, either from pills, creams, or patches, along with environmental hormones, they can create hormone imbalance if proper monitoring does not occur. Or conversely, when hormones are added in the correct dose and form, hormone harmony can hap-pen. Hormone balance can also be achieved with optimal nutrition and lifestyle changes.
There are times when the body’s regulating mechanisms do not function properly, and hormone imbalances do occur. Stress factors, poor nutrition, weight gain, and transitional times such as puberty and menopause have a tremendous effect on the endocrine system’s ability to maintain hormone balance. For example, a woman who has not taken care of herself during her 30s and 40s may find that her adrenal glands are so exhausted that they cannot make her a good supply of estrogens when her ovaries retire at menopause. Or pregnancy may overwhelm the thyroid, and a woman may suffer postpartum depression or hair loss.
Each endocrine organ or gland secretes specific hormones that help maintain balance in the body by changing the activities of the cells of an organ or of cells in groups of organs; or the hormone may directly affect the activities of all the cells in the body. In the next chapter, we will outline what the steroid hormones—the sex hormones—are and what they do.

No matter where we are in terms of our health — whether we are taking proactive, preventive steps, whether we have suffered a heart attack, whether we have had heart surgery or live with congestive heart disease — our emotions and mental state affect our heart health.
Depression sufferers are four times more likely to develop heart disease. Some suggest this because people with depressive personalities are less likely to exercise regularly or have the capacity to seek out stress reduction and mind-body healing strategies. Others favour biochemical explanations because there is a connection between psychosocial stress factors such as how we think, feel and react to the perceived threats in our life. Psychosocial stress can be defined as an imbalance between the demands placed on us and our ability to handle those demands.
A 2018 Australian study that found that in a group of 221,677 adults 45 and older, those with high or very high psychological distress were at increased risk of stroke and heart attack in comparison to those with low psychological stress even when risks due to heart harmful lifestyle behaviours were accounted for.
Women More At Risk
Research shows that women are more vulnerable to depression than men. About twice as many women suffer from this affliction, a statistic echoed in most countries around the world regardless of ethnic, racial and economic situations. A combination of uniquely feminine factors put women more at risk.
Biologically, female hormones are intricately entwined with their emotions. Menstruation, pregnancy, postpartum ‘baby blues’, perimenopause and menopause — these are just a few specific situations in a woman’s life when hormonal chemical messengers can cause major mood fluctuations. Socially and culturally, women are also under strain from the multiple roles they play (wife, mother, career woman, house keeper, chauffeur), while an often relatively lower income puts women more at risk of depression.
If you think depression is affecting you, sharing this concern with a trusted professional is important. In a 2003 National Women’s Health Resource Center survey of more than 1,000 women, although the majority reported having been depressed or having known someone with depression, almost half would not discuss matters with a health-care practitioner. This is doubly and tragically ironic considering 95 percent of them also understood that depression is treatable. As it stands, many people with depression are not adequately treated and, in women, depression is misdiagnosed 30 to 50 percent of the time.
Men and a Missed Diagnoses
Depression also affects men and current statistics may not accurately capture rates in men due to higher rates of misdiagnosis. Men may not recognize symptoms, or may ignore and downplay the symptoms they are having. Even if they are aware there is a problem, they may be reluctant to seek help or discuss their symptoms with a health car professional. Men are more likely to die from suicide, suffer addiction, and often have less access to social support systems or to seek social support.
Symptoms of Depression
- Change in appetite leading to weight gain or loss
- Concentration or memory troubles
- Crying easily or unexplained crying
- Feeling like you are pushing yourself through the day
- Feeling numb emotionally, perhaps even to the point of not being able to cry
- Feeling restless but not being able to relieve those feelings
- Feeling sad or empty
- Feeling tired all the time
- Feeling worthless or guilty
- No interest or pleasure in things you used to enjoy
- Problems sleeping, especially in the early morning, or wanting to sleep all the time or ‘hide under the covers’
- Thinking about death or suicide
- Trouble making everyday decisions
Symptoms of Depression that May Be Seen in Men
- Avoidance behaviour (escaping from uncomfortable or difficult thoughts and feelings)
- Increased anger or irritability
- Reduced sex drive or ability to preform
- Risky behaviour
- Social isolation
- Substance abuse
- Suicidal thoughts
- Violent behaviour
Achy, Breaky Heart
When we are depressed, the nervous system is stimulated and puts stress on the heart. Heart rate and blood pressure increase and the risk of irregular heartbeat (arrhythmia) rises. Depression causes dysfunction of our ‘happy hormone’ serotonin, which encourages blood platelets to clump together, creating blood clots that can eventually clog arteries and cause heart attacks.
People with depression have more heart attacks and are more likely to die of sudden death. In one study of 2,800 heart-disease-free participants, those suffering from major depression were three times more likely to develop fatal heart disease within four years than those who were not depressed. A 2009 study in Journal of the American College of Cardiology confirmed this link, evaluating 63,000 women from the long-running Nurses Health Study (1992-2004). None had heart disease signs at the study’s beginning; eight percent showed signs of serious depression. The depressed women were over twice as likely to die from sudden cardiac death, frequently caused by arrhythmia. They were also slightly more likely to die from coronary heart disease than the women without depression.
Formulate Your Heart-Health Plan
Not only is depression a heart disease ‘precursor’, but people who have a cardiac event (like a heart attack) or who are in recovery mode (after heart surgery) are also prone to depression, which actually increases the chance of another heart attack and/or heart-disease-related fatality. Another recent study in the journal Circulation also suggests that depression further increases the risk of atherosclerotic progression (thickening of the arteries).
After a heart attack or surgery, it is crucially important to formulate a heart-health plan. Gather a supportive team comprised of healthcare advisors and family, friends, club members or someone from your religious faith—whomever you need. If depression is a part of your life, or if you think you might be depressed, your team may involve a counselor or psychologist—again, someone you feel comfortable with to help guide you to better mental and emotional health.
Lifesaving Support
Social and family life keep us healthy. People with healthier support networks report better health. Single people have higher death rates than married people. Retired men who have often given up a huge portion of their lifelong identity—their work—have almost double the risk of fatal heart attack than working men.
Men and women with poor social support are more likely to suffer complications during cardiovascular surgery. In early 1980s research, Hawaiian men with large social networks (family, work, church, social groups) were less likely to suffer a heart attack, angina or other forms of heart disease.
Interestingly, the stronger a man’s social connections, the lesser the risk. In 2003, in a review of that evidence, National Heart Foundation of Australia researchers concluded in the Medical Journal of Australia that “there is strong and consistent evidence of an independent causal association between depression, social isolation and lack of quality social support and the causes and prognosis of coronary heart disease.”
Anger Hurts the Heart
Faced with upsetting news or an unwanted situation, clenching our fists, grinding on our back teeth, and lashing out verbally, causes internal stress. Which can trigger an immediate heart attack or sudden cardiac death, but it also causes more long-term wear and tear on our cardiovascular system.
In times of anger and heightened emotions, numerous physical changes are activated. We tense up as if preparing for battle. Cortisol, a ‘stress’ hormone, surges through our system. Our heartbeat speeds up and our arteries constrict, raising our blood pressure, triglycerides and cholesterol. Simultaneously, our heart’s need for oxygen to sustain these changes increases. This set of factors is why angina (chest pain) is a common symptom during bouts of anger and panic attacks. Stress, cortisol and other hormones, meanwhile, are also getting busy elsewhere in the body while, as we discussed elsewhere, the hard-working adrenal glands become exhausted.
More than 50 years ago, the propensity toward unhealthy excitable emotions and the accompanying traits of aggression, hostility, over-achievement, competitiveness and impatience was deemed Type A behavior by two cardiologists. Type As, they argued, had a higher risk of heart disease. But over time, some aspects of their theory have been rejected, others refined. Many Type As, it turns out, do quite well in life, managing their stronger personality traits without ill health effects. It is people prone to anger, hostility and cynicism who are especially vulnerable to heart disease.
Living in a state of chronically elevated stress hormones sets the stage for high blood pressure, arterial damage and atherosclerosis. In one Harvard study of 1,600 participants who had had a heart attack, eight percent reported being angry in the 24 hours prior to the attack. Those who also reported intense anger in the two hours prior had double the heart attack risk. In 2009, researchers did a meta-analysis of 44 studies on coronary heart disease and anger and hostility. These emotions, they concluded, impact heart disease outcomes in both healthy populations and in people with existing heart disease. In other words, whether we have heart disease or want to avoid it, learning to appropriately handle our emotions is essential.
Anxiety — The False Heart Attack
Poor Jack Nicholson in the film, Something’s Gotta Give. You cannot help but sympathize with his character when he suffers what he thinks is a heart attack after being rejected by Diane Keaton’s character, only to later be told by a doctor (played by Keanu Reeves) that he had had a panic attack instead.
Heart attacks and anxiety attacks have overlapping symptoms so it is easy to understand where the mistake is made. Both involve an increased heart rate and an irregular beat, and both are painful and uncomfortable. With a heart attack, however, the severity of pain is usually stronger and may affect other parts of the upper body besides the chest—the arms, jaw, neck, stomach (for other heart attack and gender specific symptoms, see Heart Disease). Heart attack victims do not tend to hyperventilate, while people having a panic attack might (unless it was the panic attack that triggered the heart attack).
Using learned techniques, such as deep breathing and relaxation exercises, panic attacks can be controlled and heart disease slowed. Anxiety sufferers may also find benefit with 5-HTP (5-hydroxytryptophan), a metabolite of the amino acid tryptophan. Proteins in the food you eat provide amino acids, including tryptophan. Tryptophan is broken down by vitamins, enzymes, and other cofactors into 5-HTP, and 5-HTP is then turned into serotonin, our “feel good” hormone. Serotonin is the neurotransmitter that tells your brain that you are satisfied and do not need to eat more. Serotonin deficiency contributes to weight gain, depression, sleeplessness, anxiety, inflammation and joint pain, among other symptoms.
5-HTP, extracted from the herb Griffonia, has been researched for the treatment of depression, anxiety and insomnia and other sleep disorders, and comes without the potential side-effects of pharmaceutical anti-depressants and sleep aids. Look for 5-HTP that is pure and enteric coated. Enteric coating ensures the 5-HTP is absorbed in the small intestine. Poor quality, non-enteric coated 5-HTP can cause nausea when taken in optimal doses.
Recommended dosage: start with 50 mg in the morning, 50 mg mid-afternoon and 50 mg at bedtime. You can go as high as 200 mg three times a day, but start with the lower dosage as it is often enough for aiding sleep and reducing anxiety. 5-HTP provides relief within two weeks, and it can be taken long-term with no side-effects. However, if you are taking MAO inhibitors, SSRIs (Prozac, Luvox, Paxil, Effexor, Zoloft) and/or tricyclic anti-depressants (Elavil, Tofranil, Pamelor), do not take 5-HTP without discussing it with your health-care provider. 5-HTP is used to wean people off SSRIs and other anti-depressants, but this should be done under the guidance of a physician.
Pets Invited
Animals are very heart-healthy. In the aftermath of a heart attack, dog owners are significantly more likely to be alive one year later, regardless of how severe the attack, according to a National Institutes of Health study involving 421 adults. In another study involving 240 married couples, those with pets had lower blood pressure and heart rates in both times of relaxation and stress, compared to non-pet owners. Owning a dog also invites more opportunities to get out there and walk, as other studies have shown. Dog owners get more exercise, resulting in other heart benefits and greater mobility.
Cats are equally as heart healthy as they too help to reduced levels of stress and anxiety. One study looked at 4,435 adults between the ages of 30 and 75, half of the group were cat owners. The study found that, over a 10 year period 5.8 percent of the non-cat owners died of heart attacks while only 3.4 percent of the cat owners died.
In addition to reducing stress and anxiety, animals have been shown to reduce depression and combat feelings of isolation and loneliness, all of which can negatively affect heart health.
The Mind is the Body
Gone are the days when heart disease was strictly considered a physical phenomena, the mind and body disassociated from each other. Thinking on this point has come full circle in the past few decades, supported by a growing body of research. Simply put, heal our minds, heal our emotions, heal our hearts. Healthy emotional expression and positive thoughts (and reactions) are part of a strong heart-health plan. We can stop destructive patterns and replace them with beneficial alternatives.
Mood-enhancing, anti-stress considerations and techniques can be found in Meditation and Inspiration. For now, though, do yourself a favor. Give yourself a moment to just breathe. Place your hands at your sides or over your stomach if you wish. If you are in bed, sit up and put your feet on the floor.
Close your eyes. Focus on pulling oxygen through your nose, deep into your belly. Hold it there, at the back of your spine for a count to eight, then release.
Repeat your breathing several times, while trying to clear your mind of anything but the moment. Let the stresses of the day drain away. When you are ready, let your eyes open. How do you feel? Relaxed, refreshed?
Congratulations, you have essentially just given your cardiovascular and central nervous systems a big hug of appreciation. Maybe even better, it did not cost a cent.

Let’s face it. Stress is inevitable. But what is not inevitable is our response to it, and how this impacts our heart and our overall health.
Imagine the following scenario. You are driving to work, and you are rear-ended. You jump out of your car, shaken, annoyed, and when you see your bashed-in bumper, your temper catches hold. What follows is an unhappy confrontation with the apologetic guilty party as you exchange phone numbers, driver’s licenses and insurance information. Because you are running late, you finish up quickly, but your bad mood lasts all day.
Here is an alternative scenario involving the same car accident. When you are hit from behind, you do a self-check and realize you are uninjured. Relieved, you get out of your car and ensure that the guilty party is also all right and did not strike you because she was having a health crisis at the wheel. Your bashed-in bumper is upsetting but, you acknowledge, it could have been worse. As you exchange information with the woman, you accept her stricken apology as genuine because you have had a few close calls yourself and you can sympathize with the guilt she is clearly feeling. You finish up and drive to work, grateful that the damage is fixable and that nobody got hurt.
Clearly, these two scenarios represent different ways of thinking about and responding to the same potentially stress-inducing incident. In the former, stress and negativity get the upper hand; in the latter, increased objectivity and positivism improve an unfortunate situation. In both cases, unseen physiological effects are occurring in the body during these kinds of scenarios — and which approach do you think is healthier for the heart? You guessed it. Number two. Short term, the second type of reaction reduces the risk of a stress-induced cardiac event (heart attack, arrhythmia). Long-term, we are following a type of behavior that reduces the risk of high blood pressure and heart strain. So how do we cultivate this way of thinking, feeling and responding? Before we delve into the how’s of stress reduction and the value of relaxing, let’s discuss the whys.
Fight or Flight: Our Genetic Legacy
Powerful mechanisms such as the fight-or-flight response have evolved through time to allow the body to shift into “survival” mode so we can either fight back or escape a perceived threat. In times of stress, various hormones within the body are secreted to relay orders. In the musculoskeletal system, muscles tense up. The nervous system reconfigures to best preserve and utilize the body’s energy stores. Focus is diverted away from areas that are not immediately essential, such as the digestive system, and is diverted toward the heart and brain where adrenaline and noradrenaline speed our reaction time, heart rate, blood pressure and blood volume pumped from the heart. The heart starts to pound, breathing quickens and becomes shallow, and we may start to sweat. It is no coincidence that these symptoms match those often found during a heart attack episode. That is why acute stress has short-term and long-term implications for cardiovascular health. Stress can also trigger anxiety attacks, which are sometimes mistaken for heart attacks.
As well, other stress hormones relay messages to boost sugar, triglyceride and cholesterol levels in the blood. The blood gets sticky in case we are injured and need to form clots so we are less likely to bleed to death. The immune system responds, ready to protect us. Over the short-term, this hormonal orchestra is designed to perform effectively. Prolonged stress, however, weakens these mechanisms, reducing immunity, causing systemic wear and tear and creating a host of physical, behavioral, emotional and cognitive symptoms. Although we are probably not trying to fight off dangerous predators like our ancestors might have been, these same stress responses can occur while we are stuck in traffic jams and conference calls.
Acute Stress and Cardiovascular Health
The tragedy of 9/11 presented researchers with an opportunity to study the impact of acute stress on the cardiovascular system. Almost 2,700 Americans who had completed a web-based assessment of acute stress prior to the terrorist attacks were reassessed one, two, and three years later. The physicians found that, even after adjusting for various factors, acute stress responses to 9/11 were associated with a 53 percent increased incidence of cardiovascular ailments, including hypertension and heart problems. These findings were reported in the Archives of General Psychiatry in 2008.
We are cramming our days full of activities and events. And regardless of what kind of stress we are under, self-imposed or otherwise — be it physical, mental, emotional or financial — our body perceives it in the same way. The brain categorizes all stress as deserving a fight-or-flight response and signals hormones to act. Over the course of a normal day, we are activating our stress response repeatedly, and this is where the problems lie.
Why We Need to Relax
We could probably all name someone (or dozens) who is a compulsive overachiever, who never seem to slow down and who claim they do not know how. We may even admire them, and silently wonder why we cannot seem to get our acts together like they have. Console yourself with this knowledge: over-activity and the compulsions behind it are not heart-healthy — in fact, they are not healthy, period. Nor are they effective long-term.
Initially, stress can enhance performance, but after a certain point, you deteriorate into mental fatigue and feel overwhelmed. Your work and mental, emotional, and physical health suffer. The stress can then lead to chest pain, arrhythmia, high blood pressure, stomach problems, sleep disturbances, depression, anger, burnout, overeating, undereating, drug or alcohol abuse, relationship conflicts, social withdrawal and much more. Stress permeates all aspects of life and is inescapable. The trick is to find a healthy balance that enhances good productivity yet includes regular relaxation.
By training yourself to relax, you are allowing your body and mind a much-needed break from life’s rigors. Physiologically, relaxing slows the breathing and heartbeat, and soothes the nervous system. Oxygen requirements decrease, blood pressure eases, the vessels dilate and blood flows easier throughout the body. If stress is the poison, relaxation is the antidote — one we should be embracing whole-heartedly. Relaxing also releases endorphins which are natural mood lifters that induce a sense of well-being.
Combined with changes in diet, exercise and nutritional supplementation, stress reduction and management is a protective tool against heart disease and future cardiac events. Ironically, knowing we need to relax and allowing ourselves to relax are two very different things. True relaxation involves a passivity and patience that doesn’t come easily to many of us. Have you personally “locked in” stress. Consider your body right now. How are you sitting? Focus on your body and identify the areas where you hold tension. Your neck and back, perhaps, from hunching over a computer all day? Your abdomen? Your jaw? Are you frowning, or smiling? Muscle actually has memory that can trigger mood (frowning vs. smiling) and induce physiological changes including heart rate and breathing. Hence, de-stressing involves calming the mind and body.

Imagine two foods on a table in front of you. The first is a hardboiled egg, the second is a white cupcake with chocolate icing. How would these foods be broken down in your body? The protein-rich egg would slowly and steadily be digested without a spike in blood glucose (sugar). The pancreas would be triggered to produce normal amounts of insulin to assist glucose uptake into cells. That cellular uptake would be equally gradual, and you would experience an even energy level until the next influx of food, hopefully an equally healthy choice.
Since glucose is the main fuel for our brain (the heart’s main source is fatty acids), it is important to balance our blood sugar in a way that supplies the body’s demands. Imagine what happens when you eat the cupcake. The refined flour, void of fiber and nutrients, is used by the body in the same way as pure sugar. It hits the bloodstream quickly, demanding an influx of insulin from the pancreas, which pumps out the hormone needed to shuttle glucose into cells. The cells take a huge sugar hit, resulting in a “sugar high” that leaves you buzzing. Before you know it, that quick burst of energy is gone. You are exhausted, yet you are left craving the next sugary sweet.
Steady Sugar Destruction
The cumulative effect of unhealthy food choices is destructive. If you indulge in a steady supply of high-sugar and/or high-carbohydrate processed foods, your body systems are going to become overwhelmed. Your pancreas can get overworked and will stop producing the insulin you need. Or maybe your cells become less inclined to heed insulin’s call and slow the uptake of glucose, otherwise known as insulin resistance. One third of North Americans have some form of insulin resistance in which your fasting glucose level (the amount of sugar in your bloodstream after several hours of no food or drink) is higher than normal, but not high enough for a diabetes diagnosis. Over time, if you do not address this dangerous situation, your blood sugar and insulin will continue to rise and a type 2 diabetes diagnosis will result.
Type 1 diabetes accounts for 10 percent of cases and usually begins during childhood. In type 1 diabetics, the immune system has destroyed the beta cells of the pancreas that produce insulin, so daily insulin injections are required. Nine out of 10 cases of diabetes are of the type 2 variety, which used to be called adult-onset diabetes but is not any longer; many children and adolescents are now diagnosed with Type 2 diabetes due to overweight and obesity. Our pancreas, cells and heart can only take the stress of poor diet and lifestyle choices for so long. According to the American Diabetes Association, two out of every three people with diabetes die of some form of heart or blood vessel disease. The average type 2 diabetic lifespan is shortened by 10 to 15 years because of the cardiovascular side effects of diabetes.
Not Sweet for the Heart
It is misleading to focus solely on the “diabetic” effect on the heart. It would be more accurate to refer to the heart disease risks caused by all prediabetic states including insulin resistance, in which blood glucose levels are unnaturally high. According to a 2001 British Medical Journal study, even elevated blood glucose is a powerful predictor of heart disease.
Excess sugar in the blood damages blood vessels by contributing to the fat deposits on their walls, which, as we know, leads to atherosclerosis, blocked arteries and all too often, heart attacks and heart damage. Too much sugar also makes blood thicker and stickier, hindering the blood’s ability to deliver nutrients and oxygen to the cells. Circulation and blood flow slows — not a good thing considering how much energy and oxygen the heart needs to sustain its pumping effects.
When we have too much glucose in the blood, it triggers the liver to make more bad, very low-density lipoproteins (VLDL) that carry triglycerides (fats) in the blood and also cause free radical damage. Consequently, diabetes and other irregular blood sugar syndromes contribute to high triglycerides and increase bad cholesterol. At the same time, the amount of good HDL cholesterol in the body decreases. This combination of high triglycerides, high bad cholesterol and low good cholesterol puts us at risk for heart disease. The inflammation brigade also wants in on the action. Persistent irregular sugar regulation increases fibrinogen and C-reactive protein (CRP), higher levels of which increase artery clogging and heart attack. Type 2 diabetics are usually found to have CRP levels four times higher than those of non-diabetics.
Several gene variants increase the risk of both type 2 diabetes and coronary heart disease. For those with a genetic predisposition to these conditions, diet and lifestyle will be essential in avoiding a health crisis.
Metabolic Syndrome/Syndrome X
Metabolic syndrome, also known as syndrome X, insulin resistance syndrome, or Reaven’s syndrome, is a cluster of factors that puts people at risk for heart disease and type 2 diabetes; doubles our risk of heart attack; and multiplies our chance of developing type 2 diabetes five-fold. It is estimated that more than 30 percent of North Americans have this disorder, which is typified by a combination of three or more of the following traits and medical conditions: elevated waist circumference, high blood fats and sugar, high blood pressure and low HDL (good) cholesterol.
Sugar Speeds Aging
Yet another biochemical process related to (pre)diabetic states and heart disease — as well as premature aging — is glycation. When blood sugar binds to and chemically alters proteins and fats, damage occurs. These damaged molecules are called advanced glycation end (AGE) products and they interfere with the way cells work. They bind with collagen and make blood vessels stiff. They also promote blood clots by attracting blood platelets, encourage the oxidation of LDL cholesterol and create low-grade inflammation that promotes atherosclerosis.
Lifestyle Is the Best Drug
If you are even 15-20 pounds overweight, you could be at risk for diabetes and heart disease. Have a glucose tolerance test to determine how quickly glucose is cleared from your blood. ‘Normal’ blood values for the 75-gram oral glucose tolerance test that is used to check for type 2 diabetes are:
Fasting: 60-100 mg/dL
1 hour: <200 mg/dL
2 hours: <140 mg/dL. Between 140-200 mg/dL is considered impaired glucose tolerance (or prediabetes, when the body has become less sensitive to insulin and has to work harder to control blood glucose levels). This group is at increased risk for developing diabetes. Greater than 200 mg/dL is a sign of type 2 diabetes.
Sometimes, blood sugar problems that generate readings too low to be “diagnosed” by traditional tests go unaddressed and cause a variety of seemingly unrelated symptoms, including anxiety, fatigue, irritability and poor concentration. Tested or untested, everybody can benefit by working to keep blood sugars balanced and controlling the processes that create diabetes and related long-term complications such as kidney, eye and nerve damage.
Diabetes Prevention
In one compelling study on diabetes prevention, 3,200 non-diabetics with elevated blood sugar readings were placed into three groups: one taking a placebo, one taking a common insulin drug, and one with a lifestyle-modification program including two-and-a-half hours of exercise per week. After three years, diabetes incidence was 11 cases per 100 people in the placebo group, 8 per 100 in the drug group and 5 per 100 in the lifestyle/exercise group. In other words, while drug therapy was more effective than placebo at preventing diabetes, a change in lifestyle was the most effective. Diet and exercise intervention reduced the incidence of diabetes by 58 percent. Similar findings about lifestyle and exercise’s effect on diabetes prevention have been repeated since.
A recent study confirms that by taking steps to regulate blood sugar metabolism, we can also help stop heart disease in its tracks. More than 3,000 participants with impaired glucose tolerance were separated into three groups: one placebo group, one taking a common insulin drug, and one that underwent lifestyle modifications, including a calorie-restricted diet and moderate exercise. Over three years, tests were conducted to assess blood sugar changes and trends in risk factors for cardiovascular disease, including blood pressure, triglycerides and cholesterol levels. The researchers found that as glucose tolerance status deteriorated, cardiovascular risk factors went downhill as well. Conversely, when blood sugar regulation improved, the risk factors improved. The researchers concluded that changing your lifestyle is more effective than taking an insulin drug at improving your glucose tolerance profile and cardiovascular risk.
Clearly, heart disease and diabetes (and prediabetic states) are largely diseases created by poor choices. Let’s attack two killers with the power of an active lifestyle, supported by a healthy diet, targeted nutritional supplements, regular stress-reducing activities, and good mental/emotional health practices.

Scientists have discovered obesity genes but they are still trying to crack the code. But we already know that obesity and a tendency to be overweight can be inherited or rooted in the behavior we learn from our families. If both parents are overweight, you will have to work a little harder to change your genetic predisposition.
For children, the statistics are even more alarming. According to the National Longitudinal Survey of Children and Youth, more than a third of Canadian children aged two to eleven are overweight, and half of those are obese. More boys than girls were found to be overweight, and preschoolers fared the worst, with one in four children between the ages of two and five being obese. The Report on America’s Children, prepared by the U.S. National Institutes of Health and the U.S. Census Bureau, contains similar statistics. That is a lot of children suffering obesity, and they are not the ones buying the groceries or driving to fast-food restaurants.
We must change the way we feed our children. Aside from the health problems associated with being an overweight child, the emotional issues can be damaging. We know that overweight children are treated differently by teachers and classmates, resulting in lower self-esteem, which further exacerbates the psychological aspects of eating. I know myself that being a chubby kid was torment. No parent wants this for his or her child.
If you know you have a family history of easy fat gain, type 2 diabetes, or heart disease, you will want to ensure that you don’t eat the same way as your mom and dad. We know that it is not just our genetic makeup, the foods we choose, our hormones, or lack of exercise, but also our psychological and emotional programs, that can keep us trapped in patterns of behavior that increase our propensity to overeat and not exercise. And where do all these patterns begin?
Environment vs. Genetics
Both the foods mom ate while you were still in the womb and the foods you were fed during early childhood have an effect on the likelihood of weight problems. If a woman develops gestational diabetes during pregnancy, or smokes, her baby is at higher risk of having an increased number of fat cells. This is one reason adopted children have been found to have similar body composition and weight-management concerns as their biological parents. Babies are less likely to be obese if breastfed for over three months. Feeding children more than they can burn off through activity, can lead to more fat cells being created. These excess fat cells make losing and maintaining a healthy weight harder in adulthood. Fat cells increase through childhood and adolescence, leveling off in adulthood. Once we have a set number of fat cells we cannot decrease our numbers, we can only shrink them.
The study most often quoted on genetic factors was led by Dr. Albert J. Stunkard, a prolific researcher on the subject of obesity. He looked at 540 Danish adults who had been adopted. A comparison of height and weight overwhelmingly demonstrated that the individuals studied were more likely to have the same body weight characteristics as their biological parents than those of their adopted family. A more recent study (2010) out of the University of Helsinki found that while environment did play a bigger role during mid childhood, once adolescence is reached and through adult hood, genetics play a larger role.
According to Harvard Medical School, over 400 different genes can contribute to weight gain. However few play a very strong role. These genes influence appetite, fullness levels when eating, how fat is distributed around the body,what foods we crave, and how fast the body’s metabolism operates. The amount genes influence weight can be anywhere from 25 to 80 percent. While genetics can make weight loss harder for some people, it does not mean weight loss is not possible. However, for people whoes weight is strongly influenced by genes, professional weight loss support from a doctor, nutritionist, or fitness trainer may be required.
Passing on Your Eating Patterns
Other studies have been conducted on the metabolic rate of children. Researchers found that children of overweight parents had a lower metabolism than did the children of parents who were not overweight. We know that when diets are predominantly made up of refined carbohydrates (processed cereals, white flour, white pasta, white sugar, white rice) and low protein, the metabolic rates will reset lower in those eaters then. It makes sense that if children eat the same types of foods as their parents, they will also have similar fat-burning rates. But being overweight has more at its core than having an increased number and size of fat cells and overweight parents. Psychologists point to the patterns of behavior that send people down the fat path.
Rewards, Love, and Fat Patterns
Patterns of behavior in children are formed at an early age. Parents, other primary caregivers, and then teachers provide a framework for children about how to behave, and food is often one of the techniques used to reinforce or deter certain behaviors. Frequently children are rewarded with candies, cookies, and junk food for good behavior or to get them to stop a behavior that adults find annoying when food is used as a reward. A child looking for attention soon learns that along with that attention comes food.
In other words, the child discovers that love and feeling good are associated with eating. Most of us have experienced this, but probably never thought about it. When we are young, a warm chocolate chip cookie is often given to soothe a bad day at school. Cookies are high in sugar, which wreaks havoc on blood sugar balance and serotonin levels. When you eat sugar, your serotonin (the feel-good hormone) increases, and you feel better. Thus there is a vicious cycle of cravings and weight gain. When your mood drops, you suddenly start craving sugar-laden foods. Eating these foods causes your serotonin to increase, and you feel good, but when the serotonin level drops, you crave these foods again. Balancing your moods and maintaining normal serotonin levels can reduce food cravings and binge eating.
An Active Model
Not only do children pick up on your eating habits, they are also influenced by how active or sedentary you are. Children of active parents are more likely to be active themselves. A study done by Boston University School of Medicine “Influence of parents’ physical activity levels on activity levels of young children” concluded that children with an active mother were 2.0 times as likely to be active, children with an active father were 3.5 times as likely, and when both are active, children were 5.8 times as likely to be active.
A 2008 study out of the University at Albany School of Public Health, found that girls were more physically active if at least one parent logistically supported their daughters activities, such as attending and enrolling them in sporting events, or at least one parent set an active or athletic example.
Home Alone Syndrome
Often, both parents work and children are left to fend for themselves before and after school. In an average week most adults spend forty to fifty hours at work, fifty-six hours sleeping, thirty hours doing house-work, and twenty-one to thirty hours watching television or searching the Internet. Children between the ages of two and eleven average nineteen hours watching television, and children older than eleven spend twenty-one hours or more on average per week in front of the television. Even families with very low incomes may have on average two televisions.
What’s worse, the television sends thousands of negative messages about food. A Saturday morning T.V. stint provides dozens of different types of fattening, toxic, fast foods and negative food messages. Advertisers are encouraging our kids to eat foods that will cause heart disease, diabetes, and cancer. And these advertisers are slick. It can be hard for parents of young children to say no to determined kids who want a McDonald’s Happy Meal™ with the hot toy of the week.
Remember, you, the parent purchases the groceries and you drive the car. Your children can’t eat junk food if you refuse to buy it. The food you keep in the house should be the food the entire family is encouraged to eat. If you have a cupboard with snacks aka ‘treats’ that you, the parents, sneaks food from, or tell your children it is only as a reward. You are then setting up your kids to have an unhealthy relationship with food. You could even be encouraging closet eating or worse shame towards the types of foods consumed.
Healthy Eating Tips for Families with Children
- Remember, you purchase the groceries and you drive the car. Your children can’t eat junk food if you refuse to buy it.
- Purchase washed and cut veggies so they are ready to use when you come home from work or when you are putting lunches together. They will also be ready for kids to eat when you aren’t home.
- Don’t buy snack cakes and cookies. Instead bake healthier versions at home if possible – Almond Butter Cookies
- No soda pop or sugar-laden, artificially flavored and colored water.
- Buy a SodaStream to make fizzy water at home or start juicing at home
- On Sunday, bake lots of chicken (skinless) or boil eggs so they’re ready to eat for the next few days. Then it will be easy for you to make lunches with good, clean protein, not bologna and processed meats.
- Limit television and video games to a certain number of hours per day and certain days per week. I know parents who unplug the television before they leave for work. Others put video games under lock and key.
- Sit down with the entire family to eat supper and talk to your kids. If you can’t do this every night, then pick a couple nights a week that are mandatory family nights. Too many families are so busy that they fail to teach their children about proper eating habits.
- Play with your children—dance in your living room, go for walks, throw a ball, ride a bike, or just have fun. Spending time with your children in fun activities will stop the negative pattern of television and food consumption that most families have adopted.
- Be physically active and support your children’s activities.
- Encourage and support hobbies and interests
- Say loving words to your children every day. Tell them, “Have I told you how much I love you today?” or, “You are so smart.” And start early—most children learn patterns by five years of age. Good self-esteem is essential to a child’s psychological eating habits.

Try this experiment. Spend a few uninterrupted moments thinking about a relaxing day at the beach or your last vacation. Maybe you spent your days lazing on a towel in the sand, feeling the heat beat down, the lulling sound of waves nearby, the mood dozy, peaceful, content. All your daily troubles were far away, the only thing crossing your mind on occasion was what to eat for dinner. Even though you might not realize it, your body is right now responding to this image. Do you feel a little more relaxed, your neck muscles looser? Has a smile inadvertently formed on your face?
The things we imagine, dream about or remember (whether it is positive or negative) actually impacts our physical self on a cellular level. Many professional athletes and Olympic contenders use this technique — they envision success to help them achieve their goals. Sports psychology is a huge industry; a good sports psychologist who can guide a team to a championship is worth her weight in gold. Athletes are often famed for their mental drive. But even if we are not athletes, we can harness this mind-body connection to help us let go of stress and heal our bodies.
Visualization (mental imagery) is a powerful tool that each of us can access within ourselves. In a way, cause and effect starts in our brain. And guiding our thoughts is an important step in life, and in health. Everyone and anyone can benefit from it. Guided imagery can be practised alone, accompanied by a CD or app, or with a health professional.
Benefits of Guided Imagery:
Visualization has proven helpful in reducing pre-surgery anxiety and post-operative pain, in managing other types of pain, in reducing stress and cortisol levels, and in reducing cravings — to mention just a few of the most recent studies. Its effect on immunity is remarkable. In a recent randomized, controlled trial, for instance, 80 women with breast cancer underwent chemotherapy followed by surgery, radiotherapy and hormone therapy. Those in a mind-body intervention group were taught relaxation and guided imagery. They also kept diaries on the frequency of relaxation practice and imagery vividness. Immunological cell activity was checked 10 times over 37 weeks. Researchers found that those women who had engaged in relaxation and guided imagery had significantly higher activity levels of several key immune responses. In other words, guided imagery and relaxation enhanced the women’s anti-cancer defenses. A recent study also confirmed the benefits of using post-stroke visualization for quicker recuperation. Stroke patients who used mental imagery had significantly enhanced relearning of daily tasks and performance compared to a group who received only conventional functional rehabilitation.
Other benefits include:
- Reduces stress and anxiety
- Improves sleep
- Speeds recovery
- Decreases blood pressure
- Decreases pain
How to Visualize for Health
There is no right or wrong way to visualize, although the more senses we use, the better it seems to work. It may also help if you personalize the image you use. If you like gardening, for example, create a visualization about being in your special outdoor place, one with nature.
This visualization would work for any body part.
Step One – Choose Your Focus
On a piece of paper, create a graphic of the body part in question. For example, if you have a blocked artery, where does the blockage occur? Shade or circle the area on the paper. If your heart is weak in a specific area, do the same. Keep in mind that this is your visualization, yours and yours alone. If it is meaningful for you to visualize your heart as the red image we all grew up drawing for Valentine’s Day, that is fine. Or you might be drawn to an encyclopedic depiction of the heart in all its complicated glory, or you might ask your cardiologist for specific details to incorporate into your image. It is less important to have a perfect anatomically correct visual than it is to create one that resonates with you personally.
Step Two – Set Your Healing Goal
Now that you have your “before” image prepared, mentally create an “after” image. If you have arrhythmia, envision a steadily beating heart. If your blood pressure is too low, perhaps your image is a pulsing heart that can push blood through the system without problem. Clogged arteries? Imagine smooth arteries unlined with plaque. You get the idea. And if you do not have a specific heart problem, just visualize your version of a healthy heart. If you also want to draw the “after” image on a separate sheet of paper for reference, go right ahead.
Step Three – Relax
Warm up with a meditation exercise. This will help you to feel relaxed and stay focused on your visualization.
Step Four – Visualize Healing
Ease into your healing visualization. Envision your “before” picture transforming into your “after” picture. A popular technique is using white light. With each breath, envision yourself deeply inhaling pure, bright light. This light is healing, soothing, and pushes out all stress and “before” images as it fills you. Gradually, envision the healing light easing down your chest and congregating around your heart (or around any other injured/ troubled area). As you exhale, imagine black light (negative energy) associated with that area being emitted out of your pores, or the soles of your feet, or other exit points. Let go of all concerns, worries, tension, anxiety and fear in the black light or smoke that leaves your body and dissipates into the universe. Repeat until all blackness is gone and your “after” picture is fully in place, surrounded by clean white energy.
A healing visualization exercise can be as short as a minute or two. Always finish a visualization with several deep, diaphragmatic breaths. Slowly open your eyes and get up when you are ready. Some people also enjoy simple stretching to reaccustom the body to activity.
Deep Breathing
In ayurvedic medicine, the traditional Indian healing system, breathing represents more than just Westernized ideas of increasing lung capacity and blood oxygen. It involves a transfer of energy, a healing exchange with our environment and the greater universe. What a wonderful and appropriate concept when it comes to the health of the heart, an organ that responds to forgiveness, love, laughter, happiness, and joy.
It goes without saying that everybody breathes; without air pumping in and out of the lungs to distribute throughout the body, we would be in trouble. Yet most people do not give thought to how they breathe.
Do this quick test now. Sit comfortably on a chair. Place one hand on your chest, the other on your belly. Breathe several times. If your chest-bound hand moves more than your belly hand, you are what is known as a thoracic breather; if your belly-bound hand moves more than your chest-bound hand, you are a belly breather. Belly – or diaphragmatic – breathing is what we instinctively did as babies. Besides providing more oxygen to the system, it also allows us to expel more carbon dioxide wastes. Most of us expand our chests when we breathe, which elevates our shoulders and is, in fact, a relatively shallow way of inhaling. Better breathing — belly breathing — pushes the abdomen in and out more forcefully, pumping more oxygen into our system.
Tuning in to how we breathe requires mindfulness and practice — mindfulness in recognizing our breathing patterns and how they change (e.g. during times of stress), and the practice to correct any unhealthy ones. One advantage to deep breathing is that you can ease into it any time, any place, anywhere — and the only person who has to know is you. Whether it is during a meeting or in a disagreement with a loved one, there is no wrong time to take a moment, reflect, then purposefully adjust. This breathing mechanism also encourages us to tune in to our bodies in general. Human beings, and women in particular, often miss those subtle messages that are being sent from within.
Mindful breathing is a habit to cultivate as much as possible. Do it daily, at whatever time and in whatever form suits you. The general rule is breath in and out through your nose (not your mouth). Breathe deeply and regularly, eyes closed, with intention and inward focus. Some people find that it helps to envision the breathing as waves, encroaching and receding.
Set the Relaxation Stage
Create your special place. It could be an unused room in your house, a sunny spot in the front yard, or a cushioned corner of your bedroom. Anywhere away from the phone or TV will do. Designate this area for relaxation and use it routinely.
Comfort first. Who can relax if you are taut with tension and holding yourself upright? Choose a comfortable chair, a pillowed seat on the floor, or whatever works for you. Your clothing should be equally unconstrained.
Time it out. Insomniacs are often encouraged to create bedtime routines. Likewise for relaxation. Choose a time of day that works for you and create a relaxation routine. Do your best to stay regular, but if you cannot, do not inwardly beat yourself up about it.
Practice, practice, practice. Routine relaxation, once per day or more, will induce the best overall effect. You will become attuned to your body, mind and emotions, while simultaneously lowering your blood pressure and heart rate, and protecting against stress effects.
Forgive your wandering mind. Learning to relax is like any other skill. It takes practice. As you try to focus inwardly, you will find your mind drifting to random thoughts. Your internal self is a chatterbox. Rather than fight these spurts, allow them to form, then let them go and refocus. Accept your own role in the process. Do not judge yourself, and you will find that relaxation comes to you.
Breathing exercise 1
Close your eyes. Whisper “ha” and feel the sound as it resonates in the back of your throat.
Close your mouth and breathe in through your nose, regularly and smoothly. As you breathe in, feel the air striking the back roof of your mouth.
Exhale while silently vocalizing the “ha” sound, experiencing it resonate in your throat. Your breath should be light, unforced, like gentle snoring.
Place your hand on your belly to ensure belly breathing (versus chest breathing). On the exhale, contract your belly muscles to ensure all air is expelled.
Repeat for two or three minutes.
Breathing exercise 2
This one is great at work. Sit at your desk, your back straight, feet flat on the floor.
Eyes closed, inhale slowly and deeply, focusing on the expansion of your belly (leave your hand on your belly if necessary). As you exhale slowly through your nose, make a low humming sound in your throat.
Repeat for two to three minutes.
Breathing exercise 3
The key to this one is in the exhalation. Exhale and inhale fully as per breathing exercise 1. Then, using your abdominal muscles, exhale spurts of air at a rate of about two per second. Exhale forcefully but with control about fifteen times. If you experience discomfort, reduce the exhalations or resume your normal breathing.
Repeat three cycles interspersed with cycles of breathing exercise 1. Always finish with a full, gentle exhale, inhale, exhale.
If ever you feel dizzy, return to your normal breathing until you feel better. Always finish with a few moments of relaxing to transition back into the real world. Some people may experience a slight light headedness, so wait peacefully until it passes.
Simple Meditation Exercise
Sit somewhere quiet and peaceful where you will not be disturbed and are less likely to be distracted. Use a chair or flat pillow.
Calm your mind with a few diaphragmatic breaths. Focus on your breathing, the in and out movement of your belly.
If you prefer, mentally focus on a neutral word or phrase, e.g. Love, Live, Peace, Joy, Relax. Words to avoid include those that sound like commands, e.g. Go, Stop, Wait.
Your mind may wander, especially as you are learning your technique. Allow it to happen, then return your attention to your breathing or word.
During this time, not just thoughts but judgements, sensations, images, memories and desires might arise. Acknowledge them, accept them as part of the process, then refocus on your breathing. Without force, these random distractions will disappear by themselves.
Set an alarm clock nearby to keep you on track. Start with 5 minutes.
Gradually continue your meditation time until you are at 20 minutes.
Meditate Stress Away
You do not have to sit on a rock, or be cross-legged and bald, to meditate. The practice of meditation has evolved past old stereotypes into a modality with applications well-suited to modern life. You may recall that depression is one of several psychosocial factors that increases the risk of heart disease. In 2009, the first large clinical trial investigated the effect of psychosocial intervention on the heart. Two hundred and eight patients with heart failure were followed for a year after eight weeks of training in meditation, coping skills and support group discussion. Compared to a control group, the participants reported lower anxiety and depression, and improved symptoms of heart failure, even at the one year mark.
The combination of meditation and breathing generated positive effects in a recent randomized pilot trial involving 52 patients who did not receive pharmaceutical treatment for high blood pressure. Those who underwent eight weeks of meditation and breathing techniques “induced clinically relevant and consistent decreases in heart rate, systolic and diastolic blood pressure.” A 2006 study noted that yoga with meditation improved endothelial function in people with coronary artery disease, and that this combination resulted in significant reductions in blood pressure, heart rate and body mass index in the 33 subjects, whether they had existing heart disease or not. In a randomized, controlled trial of 103 heart disease patients, transcendental meditation for 16 weeks improved blood pressure, insulin resistance and cardiac autonomic nervous system tone compared to a control group receiving health education.