Why Walking Works
The human body is designed to walk. What better way to spend a sunny afternoon than to get outdoors, getting an aerobic workout, increasing our heart rate, increasing circulation, strengthening the heart muscle, filling our lungs with fresh air and reaping the benefits of all that oxygen? A little rain never hurt anyone either. What has really hurt many heart disease sufferers—and people with heart disease risk factors—is a sedentary lifestyle.
The benefits of walking for the heart are numerous. Moderate physical activity, including walking, cycling, and light gardening, for 30 minutes a day cuts the risk of heart disease mortality. Even 45 minutes of exercise three times a week can reduce cardiovascular risks, depression, and emotional stress better than conventional care alone.
Best of all, it is never too late to get strolling. A 2006 study in Heart reported that couch potatoes who only started exercising later in life still cut their chances of developing heart disease significantly. People aged 40-plus who got off that couch and got active lowered their risk by 55 percent compared to the still inactive. People who had been active and stayed active enjoyed a 60 percent drop in risk for coronary heart disease. In 2006, researchers also reviewed all the current literature on walking for the prevention of heart disease and its risk factors. They noted in the Journal of Women’s Health that walking cuts a woman’s risk and has beneficial effects on risk factors such as obesity, abnormal cholesterol and triglyceride levels, hypertension, and diabetes.
Physical benefits of walking:
- Decreased chances of breast cancer
- Decreased chances of prostate cancer
- Helps to improve lower back pain
- Can improve bone density
- Increased calories burned help to maintain a healthy weight
- Can reduce the activity of genes that promote obesity
- Improves function of the immune system
- Can help to reduce pain in joints
- Helps to keep blood sugar levels balanced
Mental benefits of walking:
- Helps to reduce stress
- Improves mood
- Helps to increase creativity
- Improves sleep
Easy Walking Tips
- Listen to music while walking, which will add to the mental health benefits
- Listen to podcasts or an audio book
- Join a walking group. Starting and sticking to a fitness routine is easier if you are not alone.
- Walk during work. Skip the coffee break and head outside for 15 minutes of fresh air. The amount of cardiovascular exercise you do over a day adds up. You do not have to do 45 minutes in one session. Every 15 minutes counts.
- In bad weather, walk in a nearby shopping mall.
- Buy a pedometer. Set an initial, reasonable goal for yourself, eg. 2,500 steps a day, and increase it as you achieve it.
- Schedule walks. Write them into your day timer as you would any function or meeting. If the walk is at work, what better time to brainstorm than when the blood is pumping?
- Pick a parking spot further away from the entrance of your destination.
- Take the stairs instead of the elevator; walk up the escalator.
- Take your pet for a walk. A pet’s squiggling enthusiasm is nothing but infectious.
- Walk with a family member or friend.
- If you use transit, get off a few stops early and walk the rest of the way to your destination.

While essential fatty acids (EFA) are required for good health by everyone, they are crucial during pregnancy and lactation, and the need during infancy and childhood remains high. This is beaucase docosahexaenoic acid (DHA), arachidonic acid (AA) and other EFAs are absolutely critical for nervous system, brain and retina development, as well for fetal growth.
Eating for Two
Increased EFAs are required during pregnancy for the proper development of the mammary glands, placenta and uterus and for the development of the fetus, especially during the last trimester of pregnancy. Fetal energy and nutrient demands result in a 50% or higher increase in maternal requirements for EFAs. The greatest amount of EFAs are absorbed by the fetus during the last trimester of pregnancy. This makes premature babies especially vulnerable to EFA deficiencies (in particular, an omega-3 deficiency) as they may not have had enough time to absorb adequate EFAs.
“Eating for two” should be your mantra, not only during pregnancy, but also if you are actively trying to get pregnant. The diet before pregnancy plays an important role in determining maternal EFA state. Because EFA deficiency is so commonplace, boost your EFA intake beforehand in anticipation of the extra nutritional requirements of pregnancy. Research shows that after four weeks of EFA supplementation, tissue levels of docosahexaenoic acid (DHA) increased significantly.
In a study published in 2003 in the British Journal of Nutrition, the researchers tested the hypothesis that maternal supplementation during the second and third trimesters of pregnancy enriches maternal and/or fetal DHA status. One hundred mothers received either fish oil capsules containing 400 mg of DHA/g or a fake pill from 15 weeks gestation until term. The study found that maternal DHA status was maximal in mid-trimester and declined to term at a lower rate in supplemented compared with mothers without supplementation. The researchers concluded that maternal DHA supplementation significantly increases maternal DHA status and limits the last trimester decline, aiding preferential transfer of DHA from mother to fetus.
Fetal DHA and AA need are extremely high during the last trimester because 70% of brain cell development takes place while the fetus is in the womb. The fetal liver is not mature enough to be able to metabolize shorter chain fatty acids into the long-chain omega-3s and is unable to supply sufficient EFAs until 16 weeks before birth. Therefore, to obtain sufficient levels of EFAs the fetus depends on the transport of the fatty acids from the mother across the placenta (the special organ that supplies the baby with oxygen and food from the blood).
It is important for pregnant women to have adequate amounts of EFAs in their diet to cover their own requirements plus the requirements of the growing baby. If the pregnant woman is depleted of omega-3s before pregnancy, neither the mother nor the developing baby will have adequate levels of omega-3s. DHA may be the most critical EFA since women deficient in DHA may deliver preterm babies, as well as low birth-weight babies or develop behavioural or mood disorders, including postpartum depression.
Omega-3s for Longer Gestation and Higher Birth Weight
Every year over 13 million babies are born prematurely across the world. It is important to identify modifiable causes of preterm delivery and fetal growth retardation, which are strong predictors of an infants later health and survival. There is evidence that Inuit populations, such as those from the Faroe Islands, with a high fish intake have longer gestation periods, larger babies and reduced incidence of preeclampsia compared to those populations who consume less fish.
A study published in The Lancet showed that mothers on the Faroe Islands gave birth to bigger babies than those born in Denmark, partly due to longer gestation periods. This observation is supported by data from a study where supplementation with omega-3 fatty acids (2.7 g/day) from the 30th week of the pregnancy was associated with increased gestation (four days) and higher birth weight (107 g heavier), compared to the control group receiving olive oil as a supplement.
Fish oil has been shown in randomized trials and animal experiments to have potential to delay spontaneous delivery and prevent preterm delivery, but the minimum amount of omega-3 fatty acids needed to obtain this effect remains to be determined. Researchers from Denmark set out to investigate these issues in a study of 8729 women whose seafood intake in early pregnancy was assessed by a questionnaire. They tested whether a low intake of seafood in early pregnancy was a risk factor for preterm delivery and low birth weight and whether it was associated with a lower fetal growth. The group found that 1.9% of women who ate fish at least once per week had a premature birth, but this increased to 7.1% among women who never ate fish. The researchers concluded that low consumption of fish was a strong risk factor for preterm delivery and low birth weight.
Fish for Brawny Brains
A study published in the American Journal of Clinical Nutrition found that pregnant women who ate more fish gave their babies a better chance at mature brain development. The study also found that mothers with more DHA in their blood had babies with better sleep patterns in the first 48 hours following delivery compared to those whose mothers consumed less fish. It has been hypothesized that infant sleep patterns reflect the maturity of a child’s nervous system and are associated with more rapid development in the first year of life. The omega-3 DHA, along with the omega-6, arachidonic acid (AA), are the key building blocks for healthy brain and eye development.
Mercury and Fish
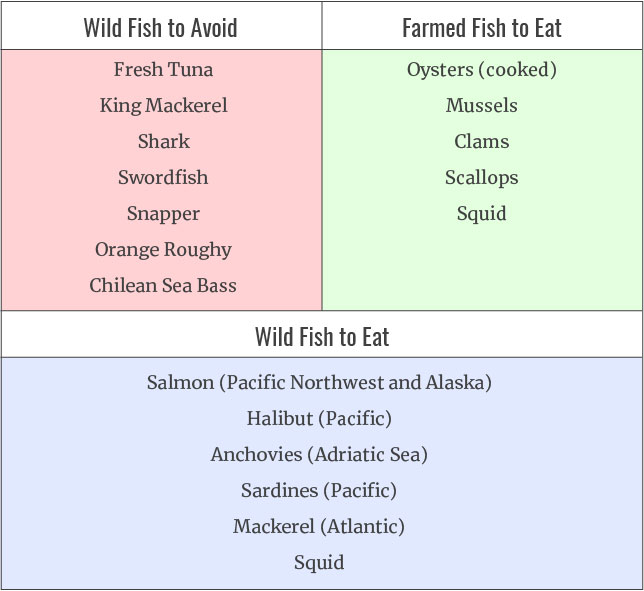
Pregnant women in North America should know that there is an increasing evidence of mercury and heavy metal poisoning in our fish supply. If they are consuming fish in their diet, they should either omit certain fish during pregnancy or reduce their intake to once every couple of weeks if they do not know the source of their fish. The safest way to consume omega-3 fatty acids without the risk of heavy metal poisoning is to consume a high quality fish oil supplements that have been tested for mercury and other heavy metals and comply with industry standards set by Health Canada. All supplements legally sold in Canada must be Health Canada approved and will have a Natural Health Product Number (NPN). Currently there is no such thing in the United States so be aware of items you buy online that are not Canadian.
One Fish, Two Fish, Bad Fish, Good Fish
Heavy metal content in longer living fish is a growing concern among health authorities. Pregnant women in particular must be careful to limit their intake to five ounces per week as dangerous elements such as mercury can pass the fetus. Farmed fish are also problematic as they are lower in omega-3 fatty acids and higher in chemicals such as pesticides, dioxins, and flame retardants. Farmed fish should be avoided with the exception of shellfish mentioned below.

Over 90 percent of hysterectomies are unnecessary. Only 10 percent of hysterectomies are deemed medically necessary.Unsuccessful conventional treatments for many common perimenopausal conditions such as heavy periods, endometrioses, uterine fibroids or prolapsed uterus put women at risk for a hysterectomy, and we feel it is important to present some information about them.
A report prepared by the Ontario Women’s Health Council says that Canadian women are having hysterectomies too frequently as a first line of treatment for discretionary reasons—to supposedly improve a woman’s quality of life—rather than to save her life. The report found that hysterectomy remains the most common procedure used to treat non-life-threatening conditions such as abnormal uterine bleeding (heavy periods), uterine fibroids, endometriosis, unexplained pelvic pain, and prolapsed uterus. And the same holds true for American women.
Just turning 40 years old in North America puts women at risk of losing their uterus. Women aged 40 to 44 years had a significantly higher rate of hysterectomy, at 11.7 per 1,000, than any other age group in the study. Fifty-two percent of all hysterectomies are performed on women younger than 44 years of age. With the population’s aging baby boomers, hysterectomy rates are only going to climb. The highest hysterectomy rate, 16.8 per 1,000, is in African American women aged 40 to 44 years.
Abdominal hysterectomies were performed more frequently than vaginal hysterectomies in all races. Hysterectomy rates are more than twice as high in northern and rural areas than in metropolitan centers that have teaching hospitals. Over 55 percent of hysterectomies also involve the removal of both ovaries, which immediately throws a woman into surgical menopause.
Female Castration
Dr. Stanley West, M.D., author of The Hysterectomy Hoax, states that “removal of the ovaries is castration. A man would never consent to having his testicles removed unless he had cancer or some other life-threatening condition, yet women have their ovaries removed in record numbers simply because doctors are not telling them they will be castrated.”
If physicians started to adopt the terminology of castration and disclosed the potential side effects of hysterectomy, most women would refuse to undergo the procedure and seek alternatives. It is important to understand how a hysterectomy may affect overall health, hormone balance, and especially the ability to have and enjoy sex afterwards.
Facts About Hysterectomy
- The word hysterectomy comes from the Greek word hystra, which means suffering caused by the uterus.
- Hysterectomy is the removal of the uterus.
- Oophorectomy is the removal of one or both ovaries.
- A complete hysterectomy is the removal of both the ovaries and the uterus.
- Supracervical hysterectomy leaves the cervix in place, which leaves the vagina longer with less discomfort during intercourse.
- Laparoscopic-assisted vaginal hysterectomy involves using a laparoscope to remove the uterus and/or ovaries.
Potential Side Effects of Hysterectomy
Although many women report that they feel better after a hysterectomy, others are not so lucky. Vaginal, abdominal, and laparoscopic hysterectomies are each performed with their own inherent risks. The reported side effects may include:
- Adhesions: Adhesions are bands of tough, fibrous, scar-like tissue that can occur during injury or surgery. These adhesions can interfere with normal functioning of an organ. Pelvic adhesions, where organs bind together, can occur on the bladder and bowel, especially if the woman has endometriosis. During a vaginal hysterectomy, the surgeon’s ability to see these adhesions may be impaired. If this happens, a woman who thought she was going to have a vaginal hysterectomy may end up with an abdominal hysterectomy.
- Bowel injury: If the bowel is accidentally cut, infection can occur, or a fistula (an opening between the rectum and vagina that allows fecal material to enter the vagina) can develop. This can be repaired during surgery, if the surgeon is aware that a cut has been made.
- Bladder injury: Infection from a cut to the bladder can occur; or a fistula between the bladder and vagina can occur, allowing urine to leak into the vagina. Again, this can be repaired during a hysterectomy if the surgeon notes the problem. This does not always happen but many women report incontinence and bladder frequency issues after hysterectomy.
- Ureter injury: The ureter is next to the cervix; it is the tube connecting the kidney to the bladder. It can be easily bruised, nicked, or otherwise injured, causing urinary tract problems.
- Ovarian failure: If the ovarian blood supply is damaged the ovaries may eventually fail after a hysterectomy. This ovarian failure following hysterectomy is seen in 15-50 percent of the cases. This is caused by impairment of ovarian vascular supply or by the loss of some important endocrine contribution by the uterus to the ovary. At surgery, effort must be made to preserve all normal ovarian tissue and prevent damage to the ovarian blood supply.
- Sexual dysfunction: Many women report never having another orgasm once they have had a hysterectomy due to important nerves being cut during the operation; others report sad feelings related to a perceived decrease or loss of their sexuality. The uterus and ovaries are a large part of what makes us female, and many women grieve the loss of their organs. (Back in the nineteenth century, hysterectomy was used as a treatment to stop perceived sexual perversions such as masturbation and promiscuity.)
- Depression and Low Libido: Estrogen acts to stimulate the release of endorphins from the hypothalamus. Removal of the ovaries (a major estrogen source) in some women has a profound effect on hormones related to happiness, resulting in mood swings and depression. The ovaries are also a source of testosterone, which promotes higher energy, vitality, and a desire for sex.
- Estrogen-deficiency symptoms: Vaginal dryness, incontinence, painful intercourse, severe hot flashes, night sweats, joint pain, heart palpitations, anxiety, and depression are reported.
- Shortened vagina: A technique called Worrelling (named after Dr. Worrell) can be used to peel the vagina away from the cervix and maintain the length of the vagina. Without this technique, many women are left with a shortened vagina and painful intercourse. Even with this technique, women have painful intercourse.
- Weight gain: Many women report a large weight gain after hysterectomy.
Think Twice About Hysterectomy
Dr. Laura Berman, Ph.D., author of The Passion Prescription states that “any surgery performed for gynecological conditions can challenge a woman’s sexual wellbeing. The medical field still does not know where all of the important nerves and blood vessels are situated in a woman’s pelvis. As a result, many are inadvertently damaged during pelvic surgeries, which can pose a real problem for sexual response. Severed nerves and blood vessels compromise lubrication, sensation, and feelings of fullness in the genital area when you are aroused.”
Some conditions require a hysterectomy due to cancer or another medically necessary reason. For all other women, use the safe, effective alternatives to hysterectomy for conditions covered in our conditions section.