In 1998 I wrote The Immune System Cure, which became a national bestseller sold in 6 countries and translated into 4 languages. In hindsight, compared to today, we knew very little about the immune system and are still discovering the broad effects of this amazing system, on our body from the brain to bone health.
A strong balanced immune system balanced is vital to preventing many common conditions we suffer today, especially if you are a woman. We know the immune system not only keeps us free from infections and cancer but is involved in conditions like allergies, sore joints, skin problems, dry eyes and mouth, Alzheimer’s, gut issues, and so much more.
Seventy-eight percent of all individuals affected by autoimmune disorders are female. Autoimmune disease results when the immune system becomes confused, and instead of attacking a virus or bacteria, it turns on the body and attacks tissues and organs. Common autoimmune diseases include rheumatoid arthritis, multiple sclerosis, Sjogren’s syndrome, psoriasis, lupus, Hashimoto’s and Graves’ thyroid disease, to name a few. When autoimmunity occurs, the immune system becomes so overactive and voracious that it can destroy body tissues.
Lack of sleep, unrelenting stress, obesity, environmental toxins, hormones, too many viral and bacterial infections all contribute to an overactive immune system. Maintaining a balanced immune system is essential to ensure the immune system protects you from invaders and controls inflammation and other negative effects of our environment.
Symptoms related to an immune system imbalance:
- Cold or flu more than once a year
- Cuts and bruises that heal very slowly
- Achy joints or muscle pain
- Digestive issues (gas, bloating, diarrhea, constipation or indigestion)
- Inflammation
- Asthma
- Skin rashes, eczema, psoriasis, hives, redness
- Allergies
- Autoimmune disease
- Parkinson’s
- Frequent urinary tract infections
- Tired or fatigued upon waking
- Chronic or extreme stress
- Elevated cortisol and C-reactive Protein
- You are over the age of 60
- Have anxiety or depression
- Brain fog and/or memory loss
I am often asked what nutrients should be taken daily to support a strong immune system. Most importantly do not take any nutrient that calls itself an immune booster. We do not want to boost the immune system – we want to balance it. Foundational nutrients for your immune system include a great multivitamin with minerals, essential fatty acids including omega 3 and borage oil, probiotics and Moducare.
I had the great pleasure of working with Professor Bouic, Ph.D., who has been researching Moducare for over 25 years. Moducare is a daily nutrient shown to keep your immune system in balance.
Just like Goldilocks and the porridge tasting event – we want an immune system that is not too hot or overactive – not too cold or weak – but most importantly, balanced and strong protecting you from the development of many health conditions.
During the pandemic, I was reminded how important Moducare is to our daily nutrient program. Moducare is a unique combination of plant sterolins and sterols in a specific ratio clinically researched for allergies, infections, inflammation, autoimmune disease and more. It is available in capsules and also a great-tasting chewable tablets for kids and adults who don’t want to swallow capsules. To learn more about Moducare, go to www.moducare.com
Knowing one’s body is an important part of staying healthy. When people are properly educated on how different systems in the body work, as well as proper terminology, they can notice and communicate potentially serious changes to a healthcare professional. The same is true for sexual health.
In 2016, a UK survey asked 1,000 British women to locate and name the vulva, vagina, cervix, uterus, fallopian tubes, and ovaries using a medical diagram showing the female reproductive anatomy. In total, two-thirds of the women failed to identify all six parts.
A 2010 American survey found that when asked to locate the vagina, 62 percent of women could not correctly do so.
The sad truth is that most girls receive inadequate health and sex education. This leads to a lot of misinformation when it comes to genitalia and the female reproductive system.
What is Normal?
Many women feel insecure about their genitalia—a lack of knowledge of what is normal leaves them feeling abnormal. One woman told us that she did not want her husband to look at her ‘down there’ because she was deformed. She thought because she had a very long labia minora that, she was not normal. We explained that Mother Nature does not provide ‘one size fits all’ when it comes to physical assets and that some women have long labia minora while others have labia minora that look like small, flat testicles. Some women have a large clitoral hood, while others have a small one. All are normal.
Knowing your sexual anatomy is important not only for general health but it is also essential when it comes to sex and pleasure.
According to the Journal of the American Medical Association, between 22 and 28 percent of women in all different age categories have never had an orgasm. However, when women are taught how their female genitalia function, they can experience this type of pleasure. So let’s understand the beautiful female anatomy. All the structures we are discussing can provide great pleasure from sexual stimulation.
Exploring Your Sexual Anatomy
Sexual Anatomy on the Outside: The Mound of Venus
Venus, the Roman goddess of love and beauty (her Greek counterpart is the goddess Aphrodite), has lent her name to the external female sexual anatomy. The “Mound of Venus” is a lovely term for the female body’s most beautiful and sacred parts.
The fact that women can bear children and nourish them tells the world how incredible the female body is, and that wonder includes female genitalia. Sadly, many women have never looked at their genitalia. It is equally sad that many women have been told this part of their body is not beautiful.
Take a mirror and get to know your genitals. We have provided a basic diagram of what the female genitalia look like, but hundreds of variations exist. Not only is this important for your sexual health, but you can also observe if you have any bumps, moles, or growths that should be evaluated.
External Genitalia
The term ‘vulva’ includes the clitoris, the labia majora, the labia minora, the perineum, the urethra, and the anus. Some women have pubic hair from the anus to the mons pubis to their thighs. Others have very little.
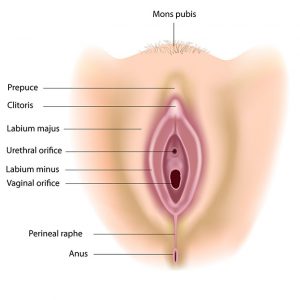
The mons pubis, also called mons venus, is the soft mound of fatty flesh over the female pubic bone. During puberty, the mons pubis becomes covered with hair. This area is rich in nerves and can be a source of sexual arousal and pleasure when stimulated, or pressure is applied.
The clitoris is a very sensitive organ that contains a high concentration of nerve endings. It is covered by the clitoral hood (prepuce). It is at the top of the labia, just above the urethra (where urine is released). The clitoris has a small head called the glans. The glans have been called the small penis. The only function of the clitoris is to provide you with pleasure.
The clitoris is an extensive organ. You can only see the small head, about the size of a pea. Still, Helen O’Connell, an Australian urologist, showed that the clitoris is quite large and extends back into the pelvis. The clitoris engorges with blood upon arousal. A healthy vascular system is just as important for women as men to ensure adequate blood flow, so an orgasm is possible. Many women have to have clitoral stimulation to achieve orgasm. Orgasms can be clitoral or vaginal. Surveys of women tend to show clitoral orgasms are more common.
The labia are composed of the labia majora, or the outer lips and the labia minora or the inner lips. Pubic hair can grow on the outer lips but not the inner lips. During arousal, the labia darken in colour and become engorged with blood. Thinning of both labia can occur due to low testosterone levels and estrogens. In severe cases, the labia majora and minora shrink and fuse together, creating a very painful condition. Aging, menopause, and hormones out of balance can also change the labia.
The perineum is the hairless area between the vagina and the anus. It is composed of an internal network of muscles. Women who have had children may have had the perineum cut (called an episiotomy) to make a larger opening for the baby’s head during delivery, or the perineum could have torn during childbirth. Some women lose sensation in this area after an episiotomy; others do not. Many women find stroking or pressure on this area quite pleasurable.
Sexual Anatomy on the Inside
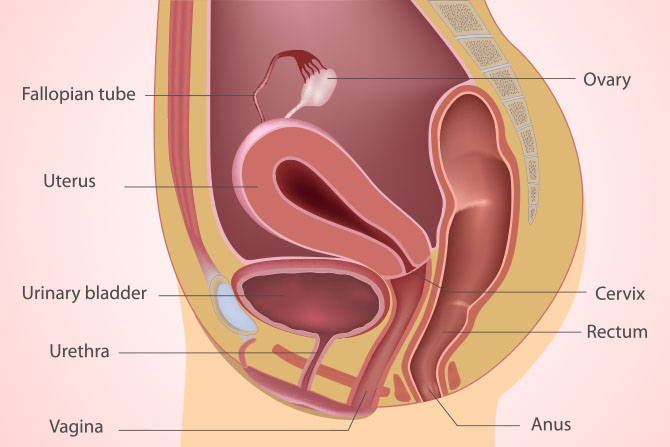
We have already discussed some female internal organs, including the ovaries, uterus, cervix, and fallopian tubes. Your vagina, and especially the G-spot, have specific sexual functions that are often overlooked in health class.
The vagina is a muscular, tube-shaped cavity leading from the vulva to the uterus. It is usually around 4 to 5 inches in length. It can expand to accommodate a penis or the passage of a baby. It can also contract and will hug or grasp a penis or tampon. The lining of the vagina is similar to the mucous membranes inside your mouth.
Lubrication occurs on the vaginal lining, keeping the vagina moist and free of bacteria. Some women notice that they are not as lubricated just after their period, childbirth, or during perimenopause and post-menopause, whereas during ovulation and sexual arousal, lubrication may be increased. Out-of-balance hormones can reduce lubrication.
Just inside the vagina is a ridge of muscles that tighten around the penis during intercourse. Most women report that they have little feeling past the outer third of the vagina.
Beverly Whipple and John D. Perry identified the G-spot (Grafenberg spot after the German physician who first suggested the presence of the G-spot). The G-spot is about the size of a bean on the front wall of the vagina (belly button side), approximately in front of the urethra. The G-spot is sensitive in some women; when stimulated, it becomes engorged and will increase to about the size of a nickel. Some women have intense orgasms when the G-spot is stimulated during sexual play. Others have never found a G-spot. Most women have a much easier time achieving orgasm through clitoral stimulation.
The Big O
During the 1960s, William H. Masters and Virginia E. Johnson (Masters and Johnson) brought sex out of the closet in their book Human Sexual Response. In their laboratory, they were the first to observe and describe a female sexual response, including orgasm. They found females responded in four phases: excitement, plateau, orgasm, and resolution.
Vaginal lubrication begins with secretions from the vaginal lining. In the excitement phase, the vagina and clitoris begin to swell. The breathing rate also increases.
During the plateau phase, the genitals become engorged with blood, causing the vaginal opening to narrow so it can grip the penis when inserted. The skin color of the labia deepens. A woman’s nipples can become erect.
The orgasm phase is achieved when the clitoris is stimulated, or enough pressure is applied to the cervix or surrounding vaginal wall to cause a build-up of tension or engorgement, eventually leading to a climax. Some women ejaculate from the urethra. Some women may think they are releasing a small amount of urine. Still, an analysis of the ejaculate revealed a chemical called acid phosphatase. Not all women ejaculate, nor is your pleasure diminished if you do not.
Orgasm is not the ultimate goal of a sexual experience. But it is a delightful, satisfying end to a time of intense pleasure with a partner or yourself. Women have told us that they do not have to have an orgasm to feel satisfied during lovemaking. However, they sometimes find it necessary to fake an orgasm so their partner is content and can ‘come.’ Other women are not sure if they have ever had an orgasm.
Men and women experience orgasms differently. You will not hear a man say, “I don’t think I have ever had an orgasm,” because their climax is easy to see. Women may have pelvic floor orgasms, clitoral orgasms, or nipple-stimulated orgasms, to name a few, and these orgasms may be intense or mild. Most men are unaware that the vagina has minimal sensation past the first third, where most nerves reside, so clitoral stimulation, along with other sexually arousing pleasures like kissing, touching, and petting, are essential for women to become excited enough for vaginal penetration. Without enough foreplay, most women will not be ready to accept the man, and intercourse can be painful.
Phases of the Female O
Resolution is a return to a non-aroused state. Some women feel alive and awake during this phase.
We must point out that no two individuals are the same. There is a complex interplay of factors involved in arousal and orgasm. For women, lovemaking is more pleasurable when foreplay and lots of stimulation are added to the mix. Both mental and physical stimulation is needed.
Inflammation, blood sugar imbalance, some viruses, and an overactive immune function are understood to play a role in Alzheimer’s disease. Ten percent of seniors over 65 have Alzheimer’s, and 50 percent of those over 85 are afflicted. With the enormous group of boomers hitting the age at the highest risk, the number affected with Alzheimer’s is expected to increase dramatically.
New evidence that the ticking time bomb in our brains is linked to the immune system suggests that an overactive immune system may be destroying neurons (neurons transmit and receive signals in the brain).
Inflammation in the brain caused by the immune system is now thought to be a significant contributor to Alzheimer’s disease. Our brains contain immune cells called microglia cells, which act like macrophages (the big eater cells of the immune system). These brain microglia cells release inflammatory immune factors like IL-6 and IL-1. Experimental animal studies and clinical trials in humans have shown that these inflammatory immune factors promote the destruction of neurons in Alzheimer’s disease brains. In certain animal studies, when IL-1 and IL-6 were blocked, the destruction of neurons was halted.
Let’s take it to the next step. Researchers worldwide have shown evidence that anti-inflammatory agents could be important in preventing Alzheimer’s. If inflammation of the brain is one of the factors that induce the destruction of neurons in the brain of someone with Alzheimer’s, then anti-inflammatory agents that cross the blood/brain barrier could halt the release of these damaging immune factors and reduce our risk of developing Alzheimer’s or halt the progression of the disease.
In both low and high doses, the curry spice curcumin reduced the inflammatory immune factors secreted by microglia cells, showing great promise for preventing Alzheimer’s. The American Medical Association suggests vitamins E, C, beta carotene and a multivitamin with minerals may help protect people against Alzheimer’s disease, postponing cognitive and memory decline.
Vitamin E and vitamin C are powerful anti-inflammatory nutrients inhibiting IL-6 and IL-1, so it makes sense that they would protect our brains from injury or immune system assault.
Many nutrients blunt the action of interleukin-1 and interleukin-6; although they have not been studied directly for their use in Alzheimer’s disease, they should also be considered excellent Alzheimer’s prevention nutrients.
These include Vitamin D3, Moducare™, and omega-3 fatty acids. Do not wait another day to start your Alzheimer’s protection program. Include these nutrients in your daily regimen.
And don’t forget to eat curry often.
References:
- Basu, A., et al. “The type 1 interleukin-1 receptor is essential for efficient activation of microglia and the induction of multiple proinflammatory mediators in response to brain injury.” Journal Neurosci (July 2002). Vol. 15:22(14) pp. 6071 82.
- Lim, G. P., Chu, T., et al. “The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse.” Journal Neurosci (Nov. 2001). Vol. 1:21(21) pp. 8370-7.
- Eikelenboom, P., Hoogendijk, W. J., et al. “Immunological mechanisms and the spectrum of psychiatric syndromes in Alzheimer’s disease.” Journal Psychiatr Res (Sept/Oct 2002). Vol. 36(5): pp. 269-80.
- Lee, Y. B., Nagai, A., Kim, S. U. “Cytokines, chemokines and cytokine receptors in human microglia.” Journal Neurosci Res (July 2002). Vol. 1:69(1) pp. 94-103.

Estrogens have a tangled relationship with food. Some foods contain estrogens and should be avoided or eaten in moderation. Some foods and herbs block estrogen; that is, they keep estrogen from fitting into estrogen receptors on cells, and some foods enhance the action of estrogen, making estrogen stronger. Some foods keep your estrogens at healthy levels by aiding the liver in detoxifying excess estrogens. Other foods stop estrogen-related cancers from gaining hold.
Phytoestrogens (phyto means plant) are naturally occurring plant estrogens that can block, increase, or detoxify estrogen. Only a limited number of plant-based foods can mimic estrogen or fit into estrogen receptors. Some phytoestrogens have no estrogen effect whatsoever, and they are estrogen-blocking.
This is why I don’t use the word phytoestrogen when talking about estrogen and plant foods. North Americans tend to have too much estrogen because estrogens are produced by the body and found in our food and environment, thereby increasing our estrogen load.
Eat plenty of these hormone-balancing foods every day. They inhibit bad estrogens and improve your estrogen-to-progesterone ratio. They are also cancer-preventing, especially cruciferous vegetables.
The Good
Eat plenty of these hormone-balancing foods every day. They inhibit bad estrogens and improve your estrogen-to-progesterone ratio. They are also cancer-preventing especially the cruciferous vegetables.
- Broccoli
- Brussels sprouts
- Cabbage
- Cauliflower
- Kale
- Kohlrabi
- Flaxseeds (ground)
- Buckwheat
- Figs
- Melons
- Green beans
- Squash
- Green tea and chamomile
Note: If you heard that cruciferous vegetables block thyroid hormone uptake, please note that you would have to eat several cups of broccoli, brussels sprouts, cauliflower, cabbage and kale every day to negatively affect your thyroid or inhibit thyroid hormones. These vegetables are super regulators of your hormone levels and should be eaten often.
The Bad
Avoid these foods altogether or limit their intake. These foods either contain estrogen, fit into estrogen receptors, or enhance the action of aromatase, an enzyme that increases estrogen. Do not eat pesticide-laden foods, as pesticides fit into estrogen receptors and increase estrogen.
- Soy beans
- Tofu
- Soy beverages
- Soy oil
- Coffee (only drink organic which is not sprayed with pesticides)
- Cotton seed oil (often found in sardines or other canned fish)
- Corn oil
- Hops in beer
- Red clover supplement
- Commercial chicken, pork or beef
- Commercial dairy products
- Farmed fish
- Alcohol

More than 100 years ago, cardiovascular disease was almost entirely a disease of men. Fifty years ago, the most popular explanations for gender-related differences in heart disease were lifestyle, including less stress for women (who were considered ‘happy homemakers’), and/ or the fact that women did not generally smoke until World War II. Today, women who have not yet reached menopause tend to have lower rates of heart disease compared to men. Postmenopausal women in North America, on the other hand, have equal rates of heart disease, with more women dying of heart attacks. Women in general also tend to have better high-density lipoprotein cholesterol levels (the ‘good’ cholesterol) and when women have higher good cholesterol, they tend to have less heart disease than men.
We have presumed for decades that women are protected from coronary disease by a built-in factor, presumably female sex hormones. This was based on the concept that all health issues in postmenopausal women have to do with declining female hormones. Several population studies suggested that a woman’s universal protection against heart disease is due to estrogen. And the medical community has perpetuated this belief because coronary heart disease is less common in women before the onset of menopause. Heart disease is more common in women who go through a premature natural menopause as well as more common in younger women who have had both ovaries removed during a hysterectomy.
Estrogen Does Not Predict Heart Disease Risk
Population-based evidence that heart disease death rates increase after menopause due to estrogen is actually weak. According to very thorough research published in the Journal of Clinical Epidemiology, there is very little evidence of a dramatic increase in heart disease due to estrogen levels in women. We do know that heart disease risk increases after menopause, but it has not clearly been shown to be to the result of declining estrogen. Researchers who do not support the theory that declining estrogen levels put women at risk of heart disease feel that estrogen may not be a primary player in heart disease development as it is for breast cancer. These researchers believe that the development of heart disease may have many factors, making it much more difficult to prove estrogen’s major role.
Some suggest that estrogen is simply not a major factor in the development of heart disease at all. In fact, there are actually no studies, according to research published in the British Medical Journal, that have shown estrogen levels in the body can predict cardiovascular disease in postmenopausal women. Estrogen levels are very poorly predicted in blood and none of the cardiovascular studies used saliva testing to get a more accurate picture of estrogen. Plus, there are many other hormones involved in heart-health protection, including testosterone and progesterone.
Hormone replacement therapy (HRT)—which generally includes synthetic conjugated equine estrogens (Premarin) and synthetic progestins like Provera (progestins are not progesterone)—has been available since the 1940s. Early observational studies suggested favorable effects in postmenopausal women using HRT. An increase in good cholesterol is seen in women using estrogen alone. And a deluge of other observational studies followed in an attempt to prove that HRT was the answer to postmenopausal coronary heart disease.
But interestingly, along the way, most studies showed an increased risk of blood clots and heart attacks in women who had just begun HRT. Then the Women’s Health Initiative study, which was designed to end the confusion once and for all about whether HRT was safe and could prevent or reduce the risk of coronary heart disease in women, was prematurely and abruptly halted in 2002 due to safety concerns. Was HRT found to be beneficial for heart disease? The answer was a resounding ‘No’ and now a paradigm shifts in the way doctors treat coronary heart disease in postmenopausal women is occurring. Let’s look at the major studies along the way.
The Coronary Drug Project
The Coronary Drug Project completed in the 1960s was the first clinical trial designed to determine whether estrogen reduced the risk of coronary events. Men with known heart disease were randomly assigned to one of five active therapies or a placebo. Two of the study medications were conjugated estrogens at a daily dose of either 2.5 or 5.0 mg; the estrogen arms were stopped early because estrogen-treated men had an increased rate of blood clots and heart attacks. After estrogen failed to protect men, no large heart-related estrogen trials were initiated in men or women for the next 23 years.
Yet despite the absence of clinical trial data, by the middle of the 1990s, it was accepted as dogma that HRT would prevent coronary heart disease in postmenopausal women. The medical profession went so far as to consider any doctor who did not recommend estrogen therapy unethical. In the wake of this, one very important researcher, Stephen B. Hulley, believed that a clinical trial showing safety and benefit in women was essential. He obtained funding for the secondary prevention trial that came to be known as the Heart and Estrogen/Progestin Replacement Study (HERS).
The HERS Trial
The HERS was the first large clinical trial designed to evaluate whether estrogen plus progestin therapy reduced the risk of coronary events in postmenopausal women who already had coronary disease.
This study, funded by Wyeth-Ayerst, was a multiple-center, randomized, double-blind, placebo-controlled trial. It included 2,763 postmenopausal women averaging 67 years of age. Each woman had an intact uterus and documented incidences of coronary heart disease. They were given a daily tablet containing conjugated equine estrogens (0.625 mg), medroxyprogesterone acetate (2.5 mg), or a placebo.
The study lasted about four years. The HERS showed no difference in coronary heart disease outcomes between the treatment and placebo groups. Non-fatal heart attacks or coronary heart disease deaths occurred in 179 women in the hormone group and 182 women in the placebo group, meaning there was no difference. This result occurred even though LDL (the bad cholesterol) decreased, and HDL (the good cholesterol) increased in the group getting HRT.
So, there was no benefit. And the really scary information is that in the first year of treatment, there was a significant 52 percent increased risk of coronary heart disease events in the group using hormones. Half of the women were followed for an additional 2.7 years and did not show any evidence of long-term cardiovascular benefit. Stroke and peripheral artery disease also did not differ between the group getting HRT and the group getting a fake pill. In other words, HRT did not make any difference and increased the risk of an adverse coronary event in the first year of treatment.
Further major studies showed an early increase in coronary death and non-fatal heart attacks in those prescribed HRT. But the medical community continued to prescribe hormones to prevent and treat heart disease. And more women died as a result.
A great debate ensued over why the trial results did not match the belief. Researchers said the women were too old or too sick. But this was not true; the average age was 67 (the average age whereby cholesterol-lowering drugs are researched). And the women were not too sick. Most had been excluded if they had had diabetes, congestive heart failure, a recent heart attack or vein disease. And over 75 percent of the women were compliant in the study. And we agree that they were prescribing the wrong hormones, including horse estrogens and synthetic progestins, which are not identical to the estrogens made by the body. The one valid criticism of the study was that it was only a single trial, possibly administering the wrong hormones. But many smaller studies also showed an increased risk of cardiac events.
By this point, significant studies showed an early increase in coronary death and non-fatal heart attacks in those prescribed HRT. But the medical community continued to prescribe hormones to prevent and treat heart disease. And more women died as a result.
The PHASE Study
In this study, a team of researchers completed an un-blinded trial with 255 women who had proven heart disease. The women, averaging 66 years of age, were either given no treatment or a 17 ß-estradiol patch (2.5 mg). No synthetic progestins were given. The patch was administered alone every four days to women without a uterus or, for women with a uterus, over 14 days, followed by four patches containing 3 mg of 17 ß-estradiol and 4 mg of norethisterone. However, the study was eventually halted due to a lack of benefits.
After approximately 31 months, it was found that there were no differences between the group receiving hormones and the group having no treatment. But the researchers found that beginning in the first year. The hormone group had higher rates of all cardiovascular events except non-fatal heart attacks. Neither an increase in good cholesterol nor a decrease in bad cholesterol was observed, and this was expected since the hormones were delivered transdermally (via the skin).
The WHI Study
The Women’s Health Initiative Study (WHI) was supposed to put to rest all concerns that arose from earlier hormone studies. This randomized, double-blind, placebo-controlled clinical trial was designed to look at coronary heart disease prevention in the form of hormone therapy, diet and calcium supplementation on disease outcomes in healthy postmenopausal women aged 50 to 79. In the hormone arm of the study, 16,608 women who had an intact uterus were randomly assigned to receive a single daily tablet containing conjugated equine (horse) estrogens (0.625 mg) and medroxyprogesterone acetate (2.5 mg) or a placebo. This was the same treatment given in the HERS. Another 10,739 women without a uterus were randomly assigned to placebo or conjugated equine estrogen (0.625 mg/d) without synthetic progestins. The study evaluated fatal and nonfatal heart disease, breast cancer, and bone health.
Even though many earlier trials showed cardiovascular risks, this trial, in particular, caught the attention of the media. After the first two-year follow-up, and then after one to two years, the Data and Safety Monitoring Board advised researchers that there was an early excess risk of heart attack and stroke in women assigned to the estrogen arms. All women were sent a letter to this effect, but most continued the treatment anyway. This is surprising considering the risk of death. In 2002, it was found that the combined estrogen-progestin arm of this study was linked to a 29 percent increase in heart attacks and a 41 percent increase in the incidence of stroke. Other adverse effects resulting from the HRT were also found, affecting the incidence of breast cancer, Alzheimer’s dementia, and even hearing loss.
The PEPI Trial and Bioidentical Progesterone
The Postmenopausal Estrogen/Progestin Interventions trial was a three-year trial involving 875 women who were perimenopausal (within 10 years of menopause). This trial was not designed to study disease outcomes.
Estrogen, when given alone, increases good cholesterol (HDL). When estrogen was given with progestins, a decline in good cholesterol was discovered. In the PEPI trial, women were given either placebo, conjugated equine estrogens, conjugated equine estrogens and synthetic progestins, either cyclical or non-cyclical, or conjugated equine estrogens and bioidentical micronized progesterone.
Of all the groups, the one receiving bioidentical progesterone had superior increases in good cholesterol. Bioidentical progesterone not only opposes estrogen’s negative effect on the uterine lining but is also very important for the heart.
Bioidentical Progesterone vs. Provera®
To protect the uterine lining from continuous stimulation by estrogen, most physicians prescribing standard estrogen repletion therapy (ERT) combine it with Provera®. If you ask if it is progesterone, you will probably even be told that it is—but it is not. It is medroxyprogesterone acetate, which is natural progesterone altered by adding a molecule to make it patentable and more orally absorbable. This molecule alters Provera’s® effect on tissues other than the uterus.
Many women discontinue ERT because they do not like how it makes them feel—irritable and often depressed. In contrast, bioidentical micronized progesterone is often called the feel-good hormone because it elevates mood and is calming. Women who have experienced mood swings and migraine headaches on Provera® notice complete resolution of these symptoms when switching to bioidentical progesterone. In addition, bioidentical progesterone was found to have the best effect on HDL cholesterol in the PEPI trial. This trial is the largest to date to include bioidentical micronized progesterone. Bioidentical progesterone can also act as a natural diuretic, in contrast to Provera®, which causes fluid retention and bloating.
There is, however, an even more compelling reason to avoid Provera®. Researchers have shown that Provera® can reverse by 50 percent the coronary-artery-dilating effect of estrogens and that bioidentical progesterone does not have this adverse effect. This evidence comes from recent studies by several different researchers and thus is unlikely to be disproved.
What Is a Woman to Do?
The WHI study has created a paradigm shift in how doctors treat heart disease. No longer is it a medical sin not to prescribe hormones to women. Now we realize that caution is needed when prescribing hormones to any woman.
If you are at risk of cardiovascular disease, do not take synthetic hormones at all—not even at a low dose for the short term. See heart disease for advice to help prevent and help treat any existing cardiovascular symptoms you may have. If you are suffering from menopausal symptoms and need relief, follow the safety advice for addressing menopausal symptoms.

The immune system is involved in promoting pain and inflammation. If the body is injured or has arthritis, for example, several chemicals and immune factors send signals to the brain that cause us to feel pain and create inflammation. If we could inhibit the release of these chemicals and factors, we would be able to control pain and inflammation.
The immune factors associated with pain and inflammation include IL-1, IL-6, IL-8, and IL-12. Carl Germano and William Cabot, in their book Nature’s Pain Killers, state that “IL-1 is directly responsible for breaking down collagen and other connective tissue increasing prostaglandin production and dilating blood vessels—all actions that create pain. IL-6 is a powerful pro-inflammatory factor that contributes to the symptoms in many painful and inflammatory conditions.”
Things That Promote the Switch to “Bad” Immunity
- Sugar suppresses certain immune cells, mainly macrophages and NK cells
- Fats containing trans fatty acids; fried foods and certain margarines suppress immunity
- Stress causes high Cortisol levels, low DHEA, suppresses immunity, and/or causes overactive immunity
- Environmental toxins, including pesticides, lead, mercury, and other heavy metals, suppress immunity and promote inflammation
- Tobacco and alcohol suppress immunity and promote high cortisol and inflammation
COX-2
Some “bad” prostaglandins also cause pain and are made from an enzyme called cyclooxygenase-2, or COX-2. The COX enzyme is actually two enzymes:
- COX-1 provides the very important function of regulating the balance of the environments in the stomach and kidneys, a type of housekeeping for the body.
- COX-2 creates prostaglandins from arachidonic acid.
Those prostaglandins generate the inflammation that causes pain. The challenge facing researchers is neutralizing the COX-2 enzyme activity without suppressing the beneficial COX-1 enzyme. While there are new COX-2 medications available that may do a good job of decreasing the inflammation and pain, they are not without side effects, such as preventing gastric ulcers from healing, inflaming colitis, and being ineffective in soothing the gastric indigestion associated with non-steroidal anti-inflammatory drug use.
Serious Side Effects from NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs), including Motrin, Ansaid, Clinoril, Neproxen, and others, are prescribed to control the pain associated with arthritis. Individuals taking NSAIDs may not be aware of the side effects. Over 20 percent will get an ulcer or gastrointestinal bleeding or even kidney and liver damage. Over 120,000 people per year are hospitalized and 18,000 die from the side effects of NSAIDs.
Joint damage is another side effect from long-term use of NSAIDs. NSAIDs cause joint destruction. Doesn’t it seem strange that you may be taking these painkillers for the pain associated with the joint destruction caused by your arthritis, but the NSAIDs prescribed by your doctor actually cause joint destruction? It is very clear in the published research. One study found that the hip joints of patients taking NSAIDs had greater joint destruction than those patients not taking NSAIDs.
New COX-2 Inhibitor Not So Safe
Celebrex, a new type of NSAID that is touted as much safer than the NSAIDs mentioned above, may not be so safe. Research performed at the University of Pennsylvania Medical Center has found that Celebrex may increase the risk of heart attack and/or stroke. Celebrex is a sulfa drug, like some antibiotics and oral diabetes drugs, so those with sulfa allergies must avoid it. Sulfa allergies affect 5 percent of the population.
Many arthritis sufferers taking Celebrex have found that the gastrointestinal problems they had with NSAIDs still occur when taking Celebrex. Simon Huang, MD, a Vancouver Rheumatologist who led local clinical trials on Celebrex, stated in the Vancouver Sun that “although Celebrex has been found to reduce ulcers in the upper GI tract the effects on the lower GI tract are unknown.”
Prednisone Has Long-Term Side Effects
Prednisone is reserved for the most serious inflammatory, allergic, and autoimmune reactions. Steroid medications like Prednisone can increase your risk of heart disease, diabetes, eye damage, severe osteoporosis, poor wound healing, weight gain, and even cancer. Use steroids as the absolute last resort.
Acetaminophen Dangers
Acetaminophen, which is used to relieve pain and is commonly sold as Tylenol, also has dangerous side effects. Unintentional overdoses are very common. If you are in severe pain, you may be tempted to take too many acetaminophen tablets. Follow the dosing recommendations carefully. Liver toxicity can occur when taking only an extra couple of doses per day. Mixing acetaminophen with alcohol causes acute liver failure. The number one cause of acute liver failure in the United States is acetaminophen overdose and misuse.
Thankfully, nature provides some exciting remedies that treat the cause of pain and inflammation.

Breast Self-Examination
Breast Self-Examination (BSE) does not prevent cancer, but many women discover abnormalities in their breasts during regular home testing. Perform the exam the day after your period ends each month. Or, for non-menstruating women, pick the same day each month. Follow these instructions to perform your self-examination:
- Lie down and put a pillow under your right shoulder. Place your right arm behind your head.
- Use the finger pads of your three middle fingers on your left hand to feel for lumps or thickening in your right breast. Your finger pads are the top-third of each finger. Press firmly enough to know how your breast feels. Learn what your breast feels like most of the time. A firm ridge in the lower curve of each breast is normal. You can either move your fingers in a circle or up and down.
- Move around the breast the same way each time you do the examination so you are aware of any changes.
- Switch the pillow to your other shoulder, and repeat with your left breast, using the right-hand finger pads.
- Repeat the examination of both breasts while standing, with one arm behind your head. The upright position makes it easier to check the upper and outer parts of the breasts (toward your armpit). (You may want to do the standing part of the BSE while you are in the shower. Some breast changes can be felt more easily when your skin is wet and soapy.)
- Check your breasts for any dimpling of the skin, changes in the nipples, redness or swelling while standing in front of a mirror.
Mammogram
Every October, during Breast Cancer Month, national campaigns encourage you to “prevent” breast cancer by having your annual mammogram. A mammogram does not prevent breast cancer. It is a diagnostic tool, albeit not the most effective one, as we are discovering.
Danish researchers reviewed seven randomized, controlled mammogram trials that supported the benefits of mammography in reducing the rate of death from breast cancer. They found that, out of the seven trials, five were so flawed they could not be considered useful; the two remaining trials also had problems. Researchers determined that mammograms had no effect on reducing deaths due to breast cancer. A study published in the Journal of the National Cancer Institute (JNCI), that followed almost 40,000 women between the ages of 50 and 59 found mammograms do not reduce the death rate from breast cancer any more than a simple breast exam.
Mammogram Concerns
The chance of receiving a false positive from mammography is substantial (meaning you have been diagnosed with cancer when there is none), according to the JNCI. Women in their 40s are at higher risk of false positives due to dense breast tissue. Women who have been taking hormone replacement therapy (estrogen and progestins) have much denser breast tissue, making it difficult to detect abnormal tissue.
A study published in the Journal of the American Medical Association found that women age 70 and older had little to no benefit from regular mammograms. The Lancet reported that breast compression, which occurs during mammography, may cause tumors to rupture, spreading cancer cells.
The safety of repeated ionizing radiation from mammograms has been questioned amid concerns that they may increase the risk of breast cancer.
What’s a woman to do?
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) of the breast does not use ionizing radiation. An MRI uses magnetic energy, not X-rays, to view the breast tissue. Multiple images of the breast are captured from many different angles and then combined using a computer to get a very detailed picture of the breast.
Researchers reported to the 39th Annual Meeting of the American Society of Oncology that MRI, by far, the highest sensitivity for diagnosing breast cancer—with the lowest rate of unnecessary biopsies. They found that MRIs provided 96.1 percent accuracy in reporting positive results, compared to mammography (42.8 percent accurate) and ultrasound (41 percent accurate). We need to insist on better detection methods.
Ask your doctor about MRI as an alternative to mammogram. Women should have a baseline breast MRI performed at 40 and then start annual MRIs at age 50.
Thermography
Another promising screening tool is thermography, which is less expensive and sometimes easier to obtain than an MRI.
In order to survive, a cancer tumor has to develop a supply of nutrients. In the early stages, it does this by stealing blood supply and nutrients from nearby cells. This process of angiogenesis continues until the blood cells form tiny capillaries that reach the tumor and start the supply of oxygen and nutrients that fuels rapid growth of the cancer. As the cancer grows, it forms a lump that can be felt during a clinical exam or seen on a mammogram, but, long before a lump is felt, heat is produced that can be detected via thermography.
All of this activity within the breast causes changes in the surface temperature of the skin. Thermography, or infrared imaging, is a non-invasive, painless technique that can indicate breast abnormalities, including benign tumors, cancer, fibrocystic breast disease, mastitis or other health issues, at very early stages. In fact, sensitive thermographic equipment is able to detect potential cancers at the stage where blood is pooling near the tumor site. Although thermography is not able to pinpoint the exact location of a tumor, it is extremely useful as a predictor of future cancer risks and, combined with other tests, could help prevent invasive tumor growth.
During the procedure, a woman sits in a cool room, and removes her clothing from the waist up. Although her skin temperature will drop and blood activity will slow, cancerous and precancerous cells are highly active and operate independently from the nervous system. As a result, these areas will continue to produce heat that will be captured by the sensitive infrared camera. Thermography is effective for detecting angiogenesis in dense breast tissue, so it is suitable for young women as well. Annual thermograms should become part of every woman’s breast health protection strategy, especially if you have decided not to have a mammogram or MRI.

The bones of the human body are constantly being broken down and rebuilt. During childhood there is more bone being made than broken down. While most of the bone mass is already created at adulthood (age 18 to 20), it may continue to grow until age 30. After this, bone mass stays quite consistent until 40, after which it starts to gradually decline in both sexes. Once women go through menopause, the loss of bone density speeds up dramatically. The higher the bone mass is at its peak, the better protected the body is against declining bone health.
Osteoporosis, or “porous bone,” occurs when bone is broken down faster than it can be rebuilt. (See Osteoporosis.) It is estimated that one in four women and one in eight men have osteoporosis. Bone fracture is a dangerous result of osteoporosis. Many people who have hip fractures as a result of osteoporosis never leave long-term care facilities. Hip fractures may result in death in up to 20 percent of cases, with men being at a greater risk of succumbing to the injury.
Bone is a matrix that contains not just bone-building minerals but also collagen, which is the protein that makes bones strong and malleable. If bone health could be attained with a simple calcium supplement, there would be a reduction in the rates of osteoporosis as women are taking calcium supplements in record numbers. But osteoporosis rates remain high and there is clearly more to strong bones than just calcium.
Exercise for Strong Muscles and Strong Bones
Bone boosting nutrients are only part of the picture and supplementation alone will not ensure strong, healthy skeletal structure. Physical activity is also essential for lasting bone health. Like the muscles, bones become stronger when subjected to the stress of weight bearing or high impact exercise; and become weaker during periods of inactivity. Ideally, a person should be active throughout their whole life; however, beginning weight bearing exercises later in life may still be helpful in avoiding osteoporosis.
Not all exercise is equal when it comes to increasing bone mass. Some examples of high-impact exercise are:
- Dancing
- Jumping rope
- Running
- Tennis
- Hiking
The above may be too much for some people; walking or using equipment like a stair stepper or treadmill are beneficial for those to run or hike.
Strength training using free weights or weight machines will also help to improve bone health.
Exercises like yoga, qi gong, and tai chi are also important as they can increase flexibility and balance which helps to protect against falls. A study from the Journal of the American Geriatrics Society in 1996 reported a 47.5% reduction in the risk of falling after following a tai chi program for 15 weeks.
Bone-Building Nutrients
Vitamin D
Vitamin D is essential for calcium absorption and is formed in the body by the sun’s rays on the skin, which then manufactures vitamin D3. Unfortunately, because people are spending more time indoors, and are wearing more sun block, deficiencies in this nutrient have risen. It is especially common during the darker months of winter and for those living at northern latitudes. Vitamin D deficiency leads to decreased calcium absorption and increased excretion of calcium via the kidneys, promoting osteoporosis and other conditions such as osteoarthritis, muscle cramps and twitching, backache and tooth decay.
Few foods contain vitamin D naturally unless they have been fortified. However, a few types of fish contain some vitamin D. Wild salmon contains the highest amount, but it is also found in trout, Ahi tuna, and mackerel in lesser amounts. Small amounts may be obtained by eating eggs from chickens able to freely roam outside (free-range).
As the body ages it is less efficient at producing vitamin D, making vitamin D supplementation essential. In addition to being necessary for optimal bone health, vitamin D is important for muscle health as strong muscles help to prevent falls. It is important to choose a supplement with the most active and powerful form of vitamin D, which is vitamin D3.
Vitamin D3 Better than D2
A 2008 study conducted by the Department of Clinical Sciences at the University of Rome, found that a single dose of vitamin D3 was almost two times as potent as D2 in increasing serum levels.
A 2010 study in the Journal of Clinical Endocrinology and Metabolism reported that in 33 healthy adults taking 50,000 IU of either vitamin D2 or D3 weekly for 12 weeks, blood vitamin D levels increased significantly more in the D3 group than in the D2 group. This clearly shows that the two forms of vitamin D, D2 (ergocalciferol) and D3 (cholecalciferol), are not absorbed by the body in the same way.
Vitamin K2, MK-7 and Bone Health
Vitamin K2, another very important bone nutrient, guides calcium into bones and locks it in. Without enough vitamin K2, calcium may lodge in places that it is not supposed to, such as in the breasts, arteries and kidneys (leading to kidney stones). Calcification occurs which causes hardening of the arteries and contributes to high blood pressure and calcium deposits in the breasts.
The “K” in vitamin K comes from the German word Koagulationsvitamin, as it was noted by researchers in Germany that this group of vitamins was essential for blood coagulation. Vitamin K1 (phylloquinone) is a blood clotting agent and acts very differently than vitamin K2 (menaquinone). Calcium in the bones and arteries is regulated by vitamin K2. Vitamin K2 is associated with osteoblasts, cells that build bone and produce a protein called osteocalcin. Osteocalcin incorporates calcium into the bones. Without vitamin K2, osteocalcin cannot be produced in the body and proteins cannot bind onto calcium without enough vitamin K2. Vitamin K2 is therefore essential to help redirect calcium into bones.
Choosing the Right Type of Vitamin K2
Vitamin K2 (menaquinone MK-7) from natto is the best form of vitamin K2. Natto is a traditional Japanese food dish derived from fermented soybeans. Other sources of K2 include liver pâté from poultry, egg yolks and dark meat from pasture-raised chickens, and butter from grass-fed cows. Half of the vitamin K that the body absorbs is from green leafy vegetables (primarily K1). Unfortunately, many foods thought to be rich in vitamin K have less vitamin K than previously assumed. Most multivitamins don’t even contain vitamin K and those that do have subpar levels. To prevent and treat osteoporosis, supplement with Vitamin K2 MK-7.
Boron
Boron is a trace mineral that helps to prevent the loss of calcium and keep bone mineralized. It also helps to prevent vitamin D deficiency by extending how long vitamin D stays in the body. Boron regulates estrogen and testosterone, which is important for postmenopausal women and their bone health. Boron may be found in raisins, nuts, beans, lentils, and dates, as well as many fruits and vegetables.
Magnesium
Magnesium is needed to convert vitamin D into its active form and absorb calcium into the bones from the bloodstream. Without magnesium, calcium will remain circulating in the bloodstream until it ends up in places it should not be found, resulting in calcium deposits around the body. Taking too much calcium can actually hinder magnesium absorption and contribute to a magnesium deficiency. Consuming the right balance of each mineral is very important and can improve bone density. The best forms of magnesium are bisglycinate and threonate; magnesium citrate should be avoided unless using for a very short time to ease constipation as this form may cause mineral imbalances.
Collagen-Supporting Nutrients for Bone Support
Another important component for bones is collagen. Over one-quarter of all the protein in the body is made up of collagen. Collagen helps make bones, nails, teeth and hair stronger. Collagen connective tissues run throughout the body and provide structure for the skeleton, tendons, cartilage and muscles, all of which support internal organs and protect softer tissues. In order to make collagen, adequate levels of protein, silicon and vitamin C must be consumed.
Silicon is a trace mineral required by the body to make collagen. Specifically, silicon is converted into silicic acid which the body requires to manufacture collagen and elastin. Unfortunately, silicon from food and herbs is poorly absorbed, resulting in a lack of the building blocks required to make collagen. Silicic acid in supplement form, on the other hand, is used directly by the body to make collagen. Silicic acid is a fabulous bone booster. Receding gums are an early indicator of osteoporosis, and some dentists have reported that supplementing with silicic acid stops receding gums.
The Best Bone-Boosting Program
To build strong bones, exercise and combine an excellent calcium/magnesium supplement that contains the right forms of calcium such as aspartate, citrate, glycinate/bisglycinate, or threonate along with:
- Boron
- Collagen-building silicic acid
- Vitamin D3
- Vitamin K2 MK-7

If you have already read my first book, The Immune System Cure, you probably have a good understanding of the immune system. This article provides more information on the developments and new discoveries in how the immune system functions and exciting new research on stress and immunity, autoimmune disease, pain and the immune system.
An Immune System Overview
Life is all about balance. Those who have discovered the joys of physical and emotional health have perfected the art of juggling work and play, exercise and relaxation, good food and junk food. On a smaller scale, even certain body functions are programmed for balance—our hormones need to be in the right ratios for optimal health, the acidity or alkalinity of the body is carefully controlled, and microscopic cells of the immune system must be in harmony or disease results.
The key to optimal health lies with our immune system. Returning balance and strength to the immune system in the face of daunting diseases like AIDS and cancer may seem very challenging. Allergies, autoimmune disease, viral infections (including herpes and human papilloma virus, the virus that causes warts and that is implicated in cervical cancer), HIV, cancer, and even heart disease are linked to a dysfunctional or imbalanced immune system.
Media reports would have us believe that boosting the immune system is the key to correcting all deficiencies, but scientists are learning that many common diseases are caused by overactive or misdirected immunity. Autoimmune disease, allergies, and inflammatory conditions like fibromyalgia and osteoarthritis are a few of the diseases where balancing immune function is more appropriate.
Immune modulation is the medical term for balancing your immune system. Intricate processes must occur in our immune system to ensure optimal function.
Little evidence is required to demonstrate how crucial the immune system is to our survival. Researchers noted that once people had recovered from some types of illness (like measles or mumps), they usually would not become infected again. It was discovered that if people survived, they developed life long protection against that specific illness.
Childhood is looked upon as immunity’s training ground, the time when this important defense system learns to recognize and fight against harmful organisms. If an infant is born with a defective immune system, the baby’s only chance of survival is to be protected in a completely sterile environment from germs of all types.
Immunity to diseases like chicken pox, measles, smallpox, and other infectious organisms is based on the production of antibodies, Y-shaped glycoproteins produced by white blood cells. This protein is programmed to kill a specific intruder or antigen (foreign matter that provokes a response from the immune system).
Antigens are attached to the surface of a virus or bacteria and form a unique structure that can be recognized only by an antibody specifically designed to identify that structure. When a different antigen is presented, its specific antibody must be produced each and every time. As we gain more and more antibodies, we develop resistance. Resistance to a specific antigen is called immunity. However, the immune system provides several methods of defense to protect us from foreign invaders.
When a foreign organ is transplanted, patients must take immunosuppressants to prevent organ rejection because the immune system is so vigilant about anything foreign in the body that it will destroy the newly transplanted organ. Immunosuppressant drugs prevent rejection, but make a person highly susceptible to infections and more serious conditions such as cancer and osteoporosis. Withdrawing the immunosuppressants can reverse the conditions, but only by sacrificing the transplanted organ.
The appearance of acquired immune deficiency syndrome (AIDS) has sparked a flurry of interest in immunology not seen since the smallpox epidemics. AIDS, a devastating disease brought about by the human immunodeficiency virus (HIV), suppresses the immune system and leaves a person so vulnerable to opportunistic infections that even minor infections can become fatal.
Immunity Starts at Birth
Healthy babies inherently benefit from the natural immunity they get from their mothers as their own immune systems mature. This innate immunity or resistance to disease begins with a response against a broad range of foreign infiltrators. The response is so subtle that you are not even aware that it is going on.
First Line of Defense
The perimeter of defense begins with the physical barrier of the skin and mucous membranes. The skin keeps bacteria and foreign particles out, excretes toxins and waste from within the body by sweating, and regulates body temperature. Mucous membranes of exposed body cavities—such as nasal passages, the eyes, the vagina, and the mouth—are vigilant in neutralizing potential invaders before they can enter. Saliva, tears, and vaginal secretions are the weapons that enable them to dilute and wash away microbes.
Think about how many times a day you touch your finger to the side of your nose, eyes, or mouth. Each time we do this we provide invaders direct entry into the inner body. The immune system protects us by making sure that all of our body fluids are rich in immune factors that destroy bacteria, viruses, parasites, and more, but what if we are dehydrated?
Water is essential. It ensures that we have fluid-rich areas that are full of potent immune factors. If we are dehydrated, those fluids and their immune factors around the eyes, nose, and mouth shrink and invaders have an open door to our bodies. Water is the least expensive and most effective virus fighter. Ensure that you drink eight glasses a day, especially in the winter when you are in your centrally heated home and the viruses are just waiting for an opportunity to gain hold.
If an invader gets past our physical barriers, then our immune system is waiting with a powerful arsenal of cells and immune factors. Have you ever gotten a piece of a thorn from a raspberry bush or rose stuck in your finger? Within a few hours the place where the thorn damaged the skin will become red and inflamed or swollen. This means that your innate immunity has launched an attack and is repairing the broken skin. In the tissues of your skin, macrophages are defending you against infection. A full-blown inflammatory response is now occurring in your finger.
Your Immunity Army
Your immune system is made up of organs including the thymus, spleen, bone marrow, lymph glands and microscopic cells that communicate with one another through chemical messengers called cytokines and they regulate many other systems of the body. The main cells include natural killer (NK) cells, T-Helper-2 cells, cytotoxic T-cells, B cells, and macrophages.
Macrophages
Macrophages are the cells that eat and digest foreign matter (macrophage literally means “big eater”). They are like Pac-Man cells that go throughout the body, eating and digesting invaders and waste products and taking pieces of those invaders and presenting them to other immune cells so they can be recognized for destruction.
When an infection occurs, the macrophages patrolling the area trap, break up, and destroy the foreigner, a process called phagocytosis. As well, macrophages release certain immune factors or chemical messengers to alert the rest of the immune system.
Unlike some immune cells that are very limited as to which microbes they can destroy, macrophages are not very picky, so they will attack a wide variety of viruses, bacteria, and old and dead cells. Although not all invaders are destroyed, this method is very effective. Some microbes, including staphylococci and tubercle bacillus, can actually kill macrophages or remain dormant for months or even years as they wait for the immune system to weaken and become vulnerable to attack. A healthy immune system, however, can stop these trouble makers in their tracks or leave them waiting dormant for their “big break” as long as we live.
Fever
Fever is another method of preventing bacteria and viruses from taking hold. Elevating the body’s temperature, even by two degrees, can hinder an invader’s progress or kill it. The phagocytes release pyrogens (a fever producing substance released by phagocytes) to induce fever. If the fever goes too high (just a few degrees or more), it can be deadly to the host. Because the window of opportunity to destroy viruses is so narrow and the ill-fated consequences lethal (death of the individual or the brain cells), immunologists are beginning to hypothesize that fever is an outmoded method of immune system defense, and that if humans survive another several thousand years, we may evolve in such a way that fever may no longer be used to kill invaders.
Inflammation
Inflammation is also a way for the body to defend itself and can be activated within seconds of an injury or invasion. The pain, redness, swelling, and heat that we feel destroys microbes, toxins, and other foreign material at the site of penetration. The blood vessels are constricted to repair damages and prevent the infection from spreading further. Following the activation of several different immune cells—including mast cells, macrophages, and T-cells—the lipids in the cell membranes are converted into inflammatory mediators that have potent effects.
There are three inflammation promoters: prostaglandin D2 (PGD2, derived from arachidonic acid), leukotrienes (also from arachidonic acid), and platelet-activating factor (PAF, produced by mast cells). Certain nutrients, such as essential fatty acids, control these inflammation promoters. For example, PAF released as a result of the immune response, has a profound effect on smooth muscle tissue in the lung, causing bronchial constriction, tightness in the chest, and wheezing, all of which are symptoms of asthma.
Remember that inflammation is necessary to heal tissues or eject an invader and becomes a problem only when it is chronic or long term. We don’t want to totally eliminate inflammation in the body or we will stop the immune system from healing damaged tissues.
The problem with some of the strong anti-inflammatory medications is that they can slow the inflammatory response to the point where the immune system cannot do proper healing or eliminate invaders.
Complement
Complement, another agent of the immune system, is a combination of 20 proteins (enzymes) that circulate in the blood acting as catalysts in antibody reactions. When an invader appears, complement releases a protein (enzyme), then another enzyme, and another in a cascade until all 20 proteins have been set in motion.
Each one of the 20 steps in the complement reaction has a particular function that happens at an appropriate phase in the process of killing invaders. The end result is that complement proteins call in a cavalry of phagocytes to the site of the inflammation and turn them into voracious eaters of the invaders.
Powerful Cancer-Fighting Cells
Natural killer cells (NK cells) are like assassins or professional hit men in that they have a little more finesse in the way they operate compared to macrophages. They destroy their attacker by penetrating its surface and releasing toxic enzymes into it. Like phagocytes, NK cells assume their own command and do not need to be told to kill invaders. However unlike antibodies, they do not have memory, so each confrontation is a new battle.
NK cells target parasites, viruses, bacteria, and fungi, but they have an extra assignment. They seek out and destroy cancerous cells on contact before they attach and develop into a tumor—in effect, they are the first strike against cancer. NK cells also attack cells infected by pathogens other than viruses. Studies evaluating cancer patients’ immune status have shown that their numbers of NK cells are drastically reduced; the lower the number of NK cells, the more severe the cancer.
An interesting characteristic of NK cells is that they release interferons, the chemical messengers or immune factors that prevent virus replication. Interferons incite aggression in NK cells and call more NK cells to join the fight, thus improving their overall killing ability.
Our immune system is incredibly intricate and sensitive to subtle changes, but it runs like a well-tuned orchestra and keeps us healthy as long as we provide it with all the tools it needs: good nutrition, supplements, relaxation, and exercise. If we have been neglectful by not getting enough nutrients or are under an excessive amount of stress, we put a dent in the armor, so when a particularly strong or determined microbe beats our immune system, we get sick.
The Thymus, a Superhero
The thymus is a flat, soft, pinkish-gray gland that sits behind the breast-bone. At birth, it is bigger than the heart. Physicians in the 1950s mistakenly believed that a large thymus was a defect in infants and used radiation to shrink it. Thankfully, this practice was stopped when they realized that a strong healthy immune system required a healthy-sized thymus gland.
The gland continues to grow until puberty when it reaches approximately 1.2 oz (34 g). As we age, it gradually shrinks, resulting in a corresponding decline in immunity. Doctors have told patients that this is a normal aging process, yet vitamins A, C, and E and the minerals zinc and selenium can enlarge even the most immune-compromised and shrunken thymus gland.
Conventional wisdom of the past dictated that a loss of immunity was to be expected through the course of aging. Aging decreases production of the hormone thymulin, which in turn decreases the production of T-cells and prevents the immune system from maturing.
We now know that the thymus is not doomed to shrink. Tarzan really knew what he was doing when he was pounding his chest. Find the curved bone in the center of your chest and gently pound it about a dozen times. Do this when you think about it throughout the day. This is a form of acupressure that stimulates the thymus gland to maintain size and the secretion of thyroid hormones.
Not Just Lymphing Along
The lymphatic system is made up of lymph fluid, lymphatic vessels, bone marrow, lymph nodes, the spleen, and the tonsils. It is involved in the elimination of toxic waste from tissues and is a crucial component of the immune system. Muscles, not the heart, pump fluid through this system. A sluggish lymphatic system is usually attributed to a lack of exercise.
If the battle against an infection is underway, the lymph glands become swollen and tender as they try to clear and clean the system. One of the best methods of cleaning the sludge out of your lymphatic system is to use a rebounder. A rebounder is a small trampoline that you bounce on for 10–20 minutes per day to get your lymphatics draining properly. It is also great exercise. Look for a rebounder at local department or fitness stores.
Immune Cells, the Last Line of Defense
Red and White Cells
Red cells and white cells reside in the blood, but only white cells are immune cells. Lymphocytes are one type of white blood cell that is born in the marrow of the long bones of the body. Upon maturity, white blood cells have two options: they can remain in the marrow to evolve into B-cells, or circulate throughout the body via the blood to the lymph until they reach the thymus gland, where they develop as T-cells.
When T-cells mature, they can differentiate between invading cells (“non-self”) and our own cells (“self”). Under normal circumstances, the immune system attacks only foreign substances or pathogens, whether they invade from outside the body or are made from within, like cancer cells. However, there are times when the immune system may become confused and attack healthy body cells.
T-Cells
T-cells are in charge of the cell-mediated responses to infection. Cell-mediated immunity is very important in fighting bacteria, yeast, viruses, fungi, and parasites (especially those pathogens residing within cells) by moving around the body on a seek-and-destroy mission. When they find invaders, the T-cells adhere to the cells and kill them. There are three main types of T-cells: T-helper cells, cytotoxic T-cells, and suppressor T-cells.
T-Helper Cells
T-helper cells, also known as T4 cells or CD4 cells, sound the sirens that an invasion has occurred and help the cytotoxic T-cells prepare for battle. They secrete protein messengers to initiate the growth, proliferation, and destructive ability of other immune cells. They also secrete proteins to raise the inflammatory response and the killing action of macrophages and NK cells. T-helper cells must signal the cytotoxic T-cells or other immune cells or else those cells cannot do their job. T-helper cells also send signals to the B-cells to produce antibodies.
Less than a decade ago immunologists discovered that we have two types of T-helper cells. T-helper cells are subdivided into T-helper-1 (Th-1) or T-helper-2 (Th-2), and each produces very different chemical messengers. A healthy immune system needs a balance of both Th-1 and Th-2 cells to be able to respond to different kinds of situations in the body.
T-Helper-1 Cells
T-helper-1 cells are the good guys. They prime the immune system by producing interleukin-2, which stimulates the cytotoxic T-cells to kill the infected cells. Interleukin-2, in turn, notifies the macrophages and NK cells to become aggressive and abundant. Th-1 cells also release gamma interferon, a potent cancer and virus-fighting factor. Most importantly, Th-1 cells regulate the Th-2 cells. A failure of the Th-1 arm of the immune system to control an overactive Th-2 is implicated in a wide variety of chronic illnesses. These include AIDS, allergies, cancer, autoimmune disorders, and more to be discussed later. In HIV’s progression to AIDS, there is a shift from Th-1 dominance to Th-2, exacerbating the disease.
Th-2 Cells
Th-2 cells are involved in the inflammatory, allergic, and antibody responses. Antibody production increases when Th-2 responds and if Th-2 is unregulated, it can cause the destruction of the “self” cells. Several of the immune factors (cytokines, the chemical messengers) released by T-helper-2 cells are involved in promoting inflammation and pain.
The Th-2 arm of the immune system becomes “bad” only when it is chronically overactive and when the Th-1 arm is suppressed. What causes our immune system to function inappropriately or to switch to “bad” immunity? Chronic stress, environmental toxins, and inadequate nutrition are the top three reasons.
If the two arms of your immune system could be balanced by enhancing Th-1 cells and decreasing the activity of Th-2 cells, many chronic diseases would disappear. Immunologists are searching for a drug that does exactly that, yet nature already supplies us with some powerful plant nutrients and nutritional supplements that accomplish the job very effectively. For optimal immunity, we want to keep our immune system in a Th-1 or “good” state while regulating Th-2 function.
Cytotoxic T-Cells
Cytotoxic T-cells (also known as killer T-cells, but I will refer to them as cytotoxic so as not to cause confusion with natural killer cells) rush to the site of the invasion and hook onto abnormal, malignant (cancerous), or infected cells. The surface receptors on cytotoxic T-cells are customized to identify specific invaders and then kill the invader directly by injecting a lethal cytokine. They also release another substance that improves the macrophages’ appetite and digestion, entices more macrophages to the site of infection, and encourages those macrophages to remain there.
Cytotoxic T-cells are similar to natural killer cells in that they discharge a toxic enzyme, but they are not the voracious eaters that NK cells are. Like NK cells, cytotoxic T-cells secrete interferons, immune factors that prevent the reproduction of viruses and enhance the killing action of the T-cells themselves. Cytotoxic T-cells are also effective against cancer cells and slow-growing bacteria such as tuberculosis.
Suppressor T-Cells
After an infection, suppressor T-cells close down some of the immune response operations. They stop the release of cytokines from cytotoxic T-cells and the production of antibodies. Suppressor T-cells help maintain the immune system’s balance until the next invasion begins. A healthy ratio of T-helper cells to suppressor T-cells is 2:1. When there are not enough suppressor T-cells, B-cells continue to produce antibodies in an unregulated fashion and throw the body into distress.
Thousands of microscopic reactions occur on a daily basis. They are quick and accurate and take place prior to any appearance of symptoms. The communication between these billions of T-cells allows us to function optimally.
Cytokines
Cytokines, or immunoregulating factors, are protein messengers with very important immune functions. They act as biochemical messengers and elicit many different responses from immune cells.
Researchers have focused on immune system enhancement to win the war on cancer. They have synthesized cytokines—such as interleukin-2, interferon, and tumor necrosis factor (TNF)—and made them available as prescription drugs. When used in very large doses as immunotherapies to treat certain cancers, these cytokines have shown some positive results. Kaposi’s sarcoma, hairy cell leukemia, and renal cell carcinoma reacted well, but unfortunately not without serious side effects, which included the suppression of bone marrow, severe weight loss, and liver damage.
Nutritional science has made progress in the field of immunotherapy, and discovered that many natural substances can increase the body’s ability to produce these cytokines without side effects.
Interleukins
At this stage of research, more than 30 interleukins (IL) have been identified. I will discuss the most common: IL-1, IL-2, IL-4, IL-6, IL-8, IL-10, and IL-12.
Interleukin-1
Interleukin-1 is a cytokine that induces fever, which, as discussed earlier, slows down pathogens or kills them. Raising the temperature only two or three degrees can be enough to do the job. Macrophages are the greatest producers of IL-1, which encourages T-cells to increase IL-2 production. Yet if macrophages are continually stimulated by using agents classified as “immune boosters,” the IL-1 that is released will eventually promote too much IL-6, which is a potent inflammatory interleukin; excessive amounts of IL-6 are implicated in many diseases.
Scientists have discovered that excessive IL-1 is associated with depression, arthritis, and many other inflammatory diseases, including fibromyalgia. IL-1 breaks down collagen and increases the bad prostaglandins, thus causing pain.
Interleukin-2
Interleukin-2, secreted mainly by T-helper-1 cells, signals natural killer cells to attack and also increases the NK cells’ killing action. It also sends a message to all T-cells to release more IL-2 as required, thus increasing their efforts to kill even more invaders. It is especially effective in enhancing immune responses against tumors. Interleukin-2 is an extremely powerful immunomodulator because it promotes the production of more T-helper-1 cells and controls overactive T-helper-2 cells.
Interleukin-4
Interleukin-4, secreted by T-helper-2 cells, optimizes the antibody production of B-cells, specifically the immunoglobulins IgG and IgE (they will be discussed a little later). IL-4 promotes the allergic response and inhibits the effect of macrophages. Research on the effects of lowering IL-4 shows that IgE antibody activity was suppressed, thus reducing allergic responses. In response to an allergen, T-helper-2 cells secrete IL-4 and then B-cells mature into plasma cells and secrete IgE antibodies. IgE then attaches to mast cells and they release histamine. Histamine causes the itchy skin, red eyes, runny nose, clogged mucous membranes, and more.
Interleukin-6
Interleukin-6 is secreted by T-helper-2 cells and stimulates antibody production in B-cells. Inflammation, allergic conditions (especially eczema), and autoimmune disorders are related to abnormal production of IL-6. In asthmatics IL-6 causes lung tissue damage that, if not controlled, can lead to reliance on steroid medications and puffers. IL-6, a powerful pro-inflammatory messenger that causes pain and massive inflammation in rheumatoid arthritis and other autoimmune disorders, is also involved in promoting osteoporosis. Certain nutrients control the action of IL-6, including plant sterols and sterolins, vitamins D and E, fish oils, glutathione, and magnesium.
Link Between Common Cold and Stress
Scientists have found a link between the cause of the common cold and stress. When we are under stress, interleukin-6 is secreted by our immune system. IL-6 is known to suppress our immune function, allowing viruses a chance to replicate and cause illness. Sheldon Cohen, MD, of Carnegie Mellon University in Pittsburgh, says the connection between psychological stress (the mind-body connection) and infection by respiratory viruses is clear. Cohen and his colleagues had established in earlier studies that stress was a risk factor for colds and flu, but could not find the direct link. Now with the confirmation that IL-6 causes immune suppression, they are confident that stress reduction will reduce the occurrence of respiratory illness.
IL-6 can also be overstimulated by excessive use of echinacea. Research performed at Bastyr University in Seattle, Washington, in 2000 set out to prove that if we took echinacea every day, we would be able to prevent or dramatically reduce the occurrence of colds and flu. Two groups were studied; one group received echinacea while the other group received a fake pill known as a placebo. After many months the research was evaluated. To the researchers’ surprise, the group that received echinacea every day had more colds and flu than the group that received the fake pill. Shocking? No.
Echinacea stimulates macrophages that then release IL-I, which in the short term has a positive effect of making more immune cells respond to invaders and makes them better killing machines. But when echinacea is given every day over a long term, it may promote IL-1 to then promote the secretion of IL-6 from Th-2 cells. IL-6, when overstimulated, promotes a cascade of inflammatory responses, the activation of antibodies, and more.
Some viruses actually use IL-6 to replicate and we do not want to enhance IL-6 in many viral infections. The German Commission E, the bible for herbs, states that echinacea should not be taken over the long term and it is contraindicated (meaning we should not take it) for autoimmune diseases and HIV. Echinacea was designed to be taken at the onset of a cold or flu or to jump-start the immune system. Take it for the duration of a cold.
Interleukin-8
Interleukin-8 is a pro-inflammatory messenger secreted by the endothelium (cells lining the internal cavities of the body), T-cells, and macrophages. When calcium is low in the blood, IL-8 acts as a translator in the communication between the parathyroid hormone and osteoclasts, telling the osteoclasts to release calcium from the bone to the blood. The secretion of too much Interleukin-8 can promote osteoporosis.
Interleukin-10
Interleukin-10 has an immunosuppressant action on T-cells, decreasing the rate of Th-1 proliferation in localized environments when the body deems that Th-2 would be more appropriate in the area. In tandem with IL-4, it influences the switch from the good Th-1 to the inflammatory Th-2. IL-10 stimulates B-cell activity.
Interleukin-12
Interleukin-12 is secreted by macrophages in retaliation against viruses or bacteria. IL-12 influences virgin T-cells to become Th-1, which is more beneficial in fighting bacteria and viruses than Th-2, which is more effective on parasites. IL-12 also encourages NK cells to release gamma-interferon and stimulate killing activity.
Interferons: The Virus Killer
Interferons are the first strike against most viruses and a very powerful one at that. There are three kinds of interferons: alpha, beta, and gamma. The alpha and beta interferons send a signal to nearby cells that a virus is in the area and if the cells become infected, they must commit suicide (called apoptosis). This act prevents the virus from replicating itself within the cell and then infecting the surrounding cells. Gamma-interferon, secreted by T-cells and NK cells, revs up the macrophages for duty and the B-cells for production of antibody IgG. As mentioned earlier, it also stimulates aggression in NK cells. Attempts to synthesize interferon have not been very successful. Synthetic prescription interferon is used in cancer, hepatitis C, and autoimmune disorders, often with poor results and severe side effects.
Tumor Necrosis Factor
When macrophages become hyperactive, they make and release the cytokine tumor necrosis factor (TNF). It induces fever, can kill some tumors and virus-infected cells, and sparks other immune cells into action. TNF can also bind to tumors that have TNF receptors on their surface and can cause a tumor to commit suicide.
Overproduction of TNF by macrophages can aggravate the joint inflammation experienced by rheumatoid arthritis sufferers. Patients in recent clinical studies who were given an antibody to deactivate the TNF showed improvement. In addition to interferon, scientists have synthesized tumor necrosis factor.
More Immune Heroes
B-Cells
Every day the body creates about a billion B-cells. Born in the bone marrow, they eventually take up residence in the lymph nodes; unlike T-cells, they are unaffected by the thymus and they do not travel around in the blood. The role of the B-cell is to produce and secrete antibodies, and each B-cell is specific to one unique antigen or invader. With a little help from T-cells, B-cells maintain antibody production against antigens. They introduce or present antigens to the T-cells, a necessary step before T-cells can do their work.
Upon finding an intruder, T-cells signal B-cells to begin producing antibodies. B-cells evolve into plasma cells, and produce millions of antibodies unique to that intruder. As antibodies are completed, they are released into the bloodstream to find an antigen and hook onto it, thereby tagging it for destruction. More than one antibody can latch onto an antigen. This can either completely inactivate the invader or at least delay it long enough for other immune cells to arrive and kill it.
Some plasma cells become the historians that memorize the invader’s antigens. These memory B-cells will live a long life so as to be available in case another invasion arises that requires the same set of antibodies. The next time around, the memory B-cells will make antibodies more quickly and will attack the invader more forcefully. The plasma cells that are not destined to become memory B-cells will die in about four or five days. During that short-lived time, however, antibodies will be released at an astounding rate of 2000 per second. Once an antigen has triggered an immune response, it is marked for life because memory cells are like elephants—they never forget.
Antibodies
The B-cells produce five classes of antibodies known as immunoglobulins (Ig): IgA, IgE, IgG, IgM, and IgD. IgD is rare and as yet its activity is not clear, so we will discuss only the first four.
IgA is ill equipped for tagging invaders in the blood, so most IgA is found in the mucous membranes, sweat, saliva, tears, and milk. It acts like a bouncer, pushing invaders completely out of the body or preventing them from entering in the first place. When babies receive IgA from their mothers’ breast milk, it goes directly to the mucosal lining of their intestines. It is needed there to fight the germs that babies ingest when they explore their world by putting things in their mouths. People with immune deficiency usually have low amounts of IgA in the gastrointestinal tract.
IgE is identified in allergic reactions. Large cells in the connective tissue called mast cells secrete histamine, a substance that facilitates allergic reactions. IgE releases the histamine and if too much histamine enters the system, as during a severe allergic reaction, it may induce anaphylactic shock that can be fatal. IgE’s protective mechanism also entails inflammatory reactions that can combat parasitic infections. Histamine is a powerful parasite-killing agent. Other inflammatory responses such as hay fever are also intended to be protective.
IgG is the most prolific antibody. It is exceptional at hooking onto pathogens and making them more appetizing for phagocytes. IgG covers microorganisms and is specifically trained to kill certain bacteria and viruses. IgG combats intracellular viruses by boring holes through cell membranes and accessing the cell’s internal contents. There are four subclasses of IgG, each with its own special abilities, so if one of them is depleted, it can seriously impair immune function. IgG is also the antibody that a mother passes on to her fetus through the placenta. This supply of IgG is enough to last until several months after birth when the baby is able to produce its own.
IgM is the antibody that B-cells make the most of when they first start out. IgM accelerates the chain reaction that complement requires to spur on the phagocytes and it also neutralizes pathogens by hooking onto them, which prevents them from infecting a host cell. IgM is a large antibody, so it can operate only in the bloodstream.
Autoimmune Disease
If something goes haywire in the production of these chemical messengers, it may lead to serious immune dysfunction and in some cases the production of autoantibodies. Autoantibodies identify and attack the body’s “self” cells. The inflammation that results is usually specific to particular areas in the body. Examples of the disorders that arise from auto-antibody production include rheumatoid arthritis, which affects the joints, and type 1 diabetes mellitus involving the destruction of beta cells of the pancreas.
North Americans have attempted to reduce fat and cholesterol in their diets for more than 30 years, but cardiovascular disease still causes over 40 percent of all deaths.
The cardiovascular system—comprising a heart, veins, arteries, some blood vessels, and blood—sounds simple enough. But when you discover a few facts—such as that the heart never rests or that in the course of an average lifetime, it could fill 100 swimming pools full of blood and will beat over 2 billion times—simple is not the adjective that comes to mind… amazing would be more appropriate.
Transportation System of the Body
Sixty thousand miles (96,000 km) of blood vessels course through our anatomical landscape—that’s two and a half times the circumference of the Earth at the equator—and is likened to a “river of health.” The name is appropriate provided that the river can flow unhindered to bring foodstuffs to the cells (nutrients and oxygen) and haul away the trash (toxins and cellular wastes). However, if any routes along the river become jammed, the cells starve and die or mutate into abnormal or toxic cells and promote atherosclerosis (hardening of the arteries), and ultimately death.
As the transporter of our infection-fighting white blood cells, the cardiovascular system is crucial to the immune system. Without the nutrients delivered by blood, the immune system doesn’t have the components to mount an adequate defense against invaders. If the toxins and wastes are not removed, the immune system will be overworked in fighting deformed or abnormal cell growth in the body, in addition to its regular surveillance of external invaders. To have optimal immunity, the health and vitality of the cardiovascular system is paramount, with new research confirming a direct connection between immunity and cardiovascular disease.
A team of Canadian researchers discovered that an error in the regulation of certain immune cells that fight bacterial infections might be implicated in heart attacks and strokes. Josef M. Penninger, MD, Ph.D, an immunologist at the Amgen Institute and the Ontario Cancer Institute at Princess Margaret Hospital, and the department of Medical Biophysics at the University of Toronto, found that in some people the bacteria chlamydia causes the body’s immune system to target the heart, causing inflammation and arterial plaque buildup, which leads to heart disease and myocardial infarctions (MI), commonly called heart attacks.
Parts of the Cardiovascular System
The heart is roughly the size of a fist. When at rest, it pumps an average of 1.5 gal (5–6 L) of blood per minute. The heart is a hollow muscle consisting of two top chambers called the atria and two bottom chambers called the ventricles. The heart muscle is extremely active and contains a high number of mitochondria cellular powerhouses that produce ATP or energy, which keeps our heart pumping.
Five types of blood vessels transport blood between the heart and cells:
- Arteries
- Arterioles
- Capillaries
- Venules
- Veins
High cholesterol and bacterial infections can clog up and damage the blood vessel system. Keeping this system clear of debris is essential to longevity.
Arteries are large blood vessels that bring oxygen-rich blood from the ventricles. They are wide in diameter and have thick, elastic walls that are well suited to carrying blood at forceful pressures. There are two types of coronary arteries carrying blood throughout the body: the pulmonary circuit, which carries blood from the heart to the lungs then back to the heart, and the systemic circuit, which is the network of vessels from the heart to all areas of the body.
Before arteries reach the capillaries, they subdivide into smaller, thinner vessels called arterioles, which are thinner because as they disperse throughout the body, they don’t have to accommodate the same level of pressure as the arteries. Their declining size works as a medium for linking the arteries to the capillaries.
The capillaries are the smallest vessels in the body. They connect arterioles to the venules. Capillaries have very thin walls that transfer nutrients and oxygen to the blood and tissues, and also remove carbon dioxide. Because different tissues require varying amounts of nutrients and oxygen, the number of capillaries they have varies accordingly. Muscle needs plenty of oxygen, so its capillary network is immense. The cornea and the skin do not require as much oxygen, so they have a smaller capillary network.
The venules are the tiny vessels that act as the medium between the capillaries and the veins. Veins are larger vessels that run alongside arteries, bringing oxygen-poor blood back to the heart. In contrast to the arteries, the venous walls are not under as much pressure in their circulation so they are thinner, less muscular, and less elastic.
Blood pressure is simply the force or the push against the walls of arteries as blood courses through them. Every heartbeat pumps out blood, so the pressure inside the arteries increases; as the heart relaxes between beats, the pressure drops. Two readings are required to evaluate your blood pressure. The first and larger figure is the systolic pressure—when the heart beats. The second and smaller figure is the diastolic pressure—when the heart is at rest. A normal range for systolic pressure is between 100 and 140 and between 60 and 90 for diastolic pressure.
Blood Is Thicker Than Water
Blood is composed of liquid and solid constituents. The liquid in blood is called plasma and the solids are made up of red blood cells, white blood cells, and platelets. An average adult has roughly 4–5 qts (over 4 L) of blood in his or her body. Plasma, which is 92 percent water, is a mixture of hormones, proteins, and vitamins. It holds the platelets and blood cells in suspension.
Ninety-nine percent of your blood cells are red blood cells. Their color is attributed to the protein hemoglobin, which transports oxygen to the cells of the body. A red blood cell count is the amount of red blood cells per cubic millimeter of blood. Healthy adults can have a red blood cell count of anywhere from 4 to 6 million cells.
White blood cells are created in bone marrow and are the warriors of your immune system. They eat bacteria and can produce the antibodies that destroy infectious invaders. The cells transport immune cells via the blood to the infected area. A white blood cell count for a healthy adult is only 4000 to 10,000 cells per cubic millimeter of blood. This is the cell count that doctors monitor for signs of illness. (See The Immune System.)
Platelets are cell fragments that are less than half the size of red blood cells. They repair vessels by sticking to damaged walls and causing the blood to clot (coagulation) to prevent the blood from escaping the blood vessel, but this can also be a safety mechanism that turns disastrous when excessive stickiness occurs and promotes heart disease and stroke.