While essential fatty acids (EFA) are required for good health by everyone, they are crucial during pregnancy and lactation, and the need during infancy and childhood remains high. This is beaucase docosahexaenoic acid (DHA), arachidonic acid (AA) and other EFAs are absolutely critical for nervous system, brain and retina development, as well for fetal growth.
Eating for Two
Increased EFAs are required during pregnancy for the proper development of the mammary glands, placenta and uterus and for the development of the fetus, especially during the last trimester of pregnancy. Fetal energy and nutrient demands result in a 50% or higher increase in maternal requirements for EFAs. The greatest amount of EFAs are absorbed by the fetus during the last trimester of pregnancy. This makes premature babies especially vulnerable to EFA deficiencies (in particular, an omega-3 deficiency) as they may not have had enough time to absorb adequate EFAs.
“Eating for two” should be your mantra, not only during pregnancy, but also if you are actively trying to get pregnant. The diet before pregnancy plays an important role in determining maternal EFA state. Because EFA deficiency is so commonplace, boost your EFA intake beforehand in anticipation of the extra nutritional requirements of pregnancy. Research shows that after four weeks of EFA supplementation, tissue levels of docosahexaenoic acid (DHA) increased significantly.
In a study published in 2003 in the British Journal of Nutrition, the researchers tested the hypothesis that maternal supplementation during the second and third trimesters of pregnancy enriches maternal and/or fetal DHA status. One hundred mothers received either fish oil capsules containing 400 mg of DHA/g or a fake pill from 15 weeks gestation until term. The study found that maternal DHA status was maximal in mid-trimester and declined to term at a lower rate in supplemented compared with mothers without supplementation. The researchers concluded that maternal DHA supplementation significantly increases maternal DHA status and limits the last trimester decline, aiding preferential transfer of DHA from mother to fetus.
Fetal DHA and AA need are extremely high during the last trimester because 70% of brain cell development takes place while the fetus is in the womb. The fetal liver is not mature enough to be able to metabolize shorter chain fatty acids into the long-chain omega-3s and is unable to supply sufficient EFAs until 16 weeks before birth. Therefore, to obtain sufficient levels of EFAs the fetus depends on the transport of the fatty acids from the mother across the placenta (the special organ that supplies the baby with oxygen and food from the blood).
It is important for pregnant women to have adequate amounts of EFAs in their diet to cover their own requirements plus the requirements of the growing baby. If the pregnant woman is depleted of omega-3s before pregnancy, neither the mother nor the developing baby will have adequate levels of omega-3s. DHA may be the most critical EFA since women deficient in DHA may deliver preterm babies, as well as low birth-weight babies or develop behavioural or mood disorders, including postpartum depression.
Omega-3s for Longer Gestation and Higher Birth Weight
Every year over 13 million babies are born prematurely across the world. It is important to identify modifiable causes of preterm delivery and fetal growth retardation, which are strong predictors of an infants later health and survival. There is evidence that Inuit populations, such as those from the Faroe Islands, with a high fish intake have longer gestation periods, larger babies and reduced incidence of preeclampsia compared to those populations who consume less fish.
A study published in The Lancet showed that mothers on the Faroe Islands gave birth to bigger babies than those born in Denmark, partly due to longer gestation periods. This observation is supported by data from a study where supplementation with omega-3 fatty acids (2.7 g/day) from the 30th week of the pregnancy was associated with increased gestation (four days) and higher birth weight (107 g heavier), compared to the control group receiving olive oil as a supplement.
Fish oil has been shown in randomized trials and animal experiments to have potential to delay spontaneous delivery and prevent preterm delivery, but the minimum amount of omega-3 fatty acids needed to obtain this effect remains to be determined. Researchers from Denmark set out to investigate these issues in a study of 8729 women whose seafood intake in early pregnancy was assessed by a questionnaire. They tested whether a low intake of seafood in early pregnancy was a risk factor for preterm delivery and low birth weight and whether it was associated with a lower fetal growth. The group found that 1.9% of women who ate fish at least once per week had a premature birth, but this increased to 7.1% among women who never ate fish. The researchers concluded that low consumption of fish was a strong risk factor for preterm delivery and low birth weight.
Fish for Brawny Brains
A study published in the American Journal of Clinical Nutrition found that pregnant women who ate more fish gave their babies a better chance at mature brain development. The study also found that mothers with more DHA in their blood had babies with better sleep patterns in the first 48 hours following delivery compared to those whose mothers consumed less fish. It has been hypothesized that infant sleep patterns reflect the maturity of a child’s nervous system and are associated with more rapid development in the first year of life. The omega-3 DHA, along with the omega-6, arachidonic acid (AA), are the key building blocks for healthy brain and eye development.
Mercury and Fish
Pregnant women in North America should know that there is an increasing evidence of mercury and heavy metal poisoning in our fish supply. If they are consuming fish in their diet, they should either omit certain fish during pregnancy or reduce their intake to once every couple of weeks if they do not know the source of their fish. The safest way to consume omega-3 fatty acids without the risk of heavy metal poisoning is to consume a high quality fish oil supplements that have been tested for mercury and other heavy metals and comply with industry standards set by Health Canada. All supplements legally sold in Canada must be Health Canada approved and will have a Natural Health Product Number (NPN). Currently there is no such thing in the United States so be aware of items you buy online that are not Canadian.
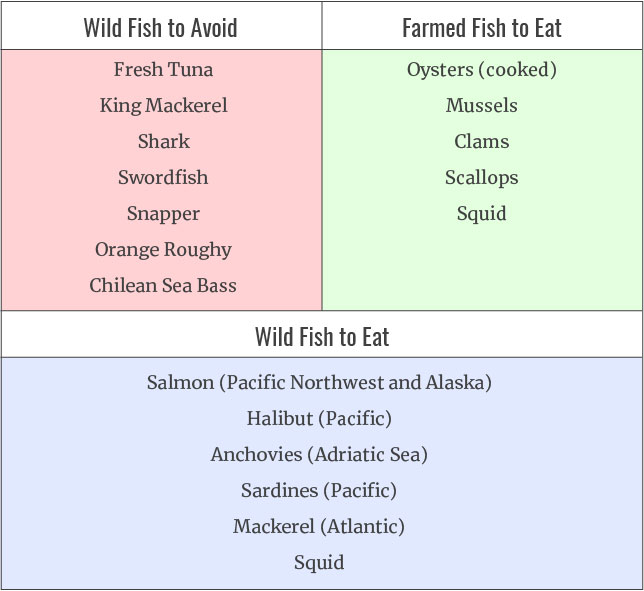
One Fish, Two Fish, Bad Fish, Good Fish
Heavy metal content in longer living fish is a growing concern among health authorities. Pregnant women in particular must be careful to limit their intake to five ounces per week as dangerous elements such as mercury can pass the fetus. Farmed fish are also problematic as they are lower in omega-3 fatty acids and higher in chemicals such as pesticides, dioxins, and flame retardants. Farmed fish should be avoided with the exception of shellfish mentioned below.