Overview
Symptoms
Causes
Prescription
Health Tips
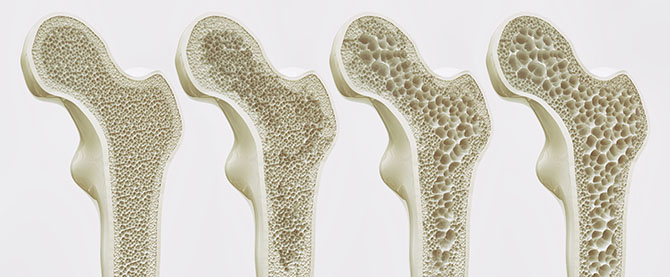
Osteoporosis (low bone density or diminished bone building) affects almost 200 million people worldwide and over 80 percent are women. One in four women and one in eight men have osteoporosis. People typically reach maximum bone mass in their early to mid 20s. After about 30 years of age, bone mass slowly starts to decrease. The greater bone density is at its peak, the better protected one is from osteopenia (low bone mineral density) and osteoporosis.
Bones are living tissue and in a constant state of regeneration as bone material is continuously broken down and rebuilt. Hormones, the liver, kidneys and immune system all work together to ensure that bone is maintained. Osteoporosis, meaning “porous bone”, arises when bone is broken down faster than it can be rebuilt. Over time a gradual decrease in bone mass and loss of bone tissue causes the bones to become porous, brittle and fragile, increasing a risk of fracture. Bones of the hips, spine, wrists and ribs are the most common fracture sites.
Hip fractures are a dangerous result of osteoporosis. It is estimated that 1.6 million hip fractures occur each year, and over 50 percent will result in some form of disability, with many patients never leaving long-term care facilities. While fractures occur more often in women, mortality rates due to hip fractures are higher in men, resulting in death in up to 20 percent of cases.
If several of the risk factors mentioned below occur, a dual-energy absorptiometry (DEXA) scan should be performed to determine bone density status.
Symptoms
Bone loss occurs silently and often symptoms are not noted until a fracture occurs. Warning signs of osteoporosis include:
- Back pain around the bottom of the shoulder blades
- Bones may fracture with little stress
- Collapsing vertebrae can pinch nerves causing sciatica
- Loss of height and a rounding of the upper back or dowager’s hump
- Pain is relieved with heat but aggravated by lying flat on the back
- Teeth may become loose
Causes
The media reports lead some to believe that calcium loss is the only cause of osteoporosis and that simply taking doses of calcium would solve the problem. Unfortunately, this is not true – calcium alone will not reverse or halt bone loss in most cases. Actually, studies using calcium alone have shown bone loss, not bone gain. Hormones, our immune system, stress reduction, physical activity and good nutrition combine to maintain proper bone health.
Low Stomach Acid
People with low stomach acid will have a difficult time absorbing calcium carbonate, the most common calcium used in supplements. Less than 10 percent of calcium carbonate is absorbed in those with low stomach acid. Calcium citrate, aspartate and orotate are much better absorbed. Calcium concentration in the body is controlled by several hormones (including calcitonin secreted by the thyroid gland) and is influenced by our immune system.
Vitamin D Deficiency
Vitamin D also plays an important role in the formation of bone. Vitamin D interacts with the cells of the immune system by reducing inflammatory cytokines, specifically IL-1 and IL-12. Carl Germano, RD, and William Cabot, MD, state in The Osteoporosis Solution that, “In some research circles, osteoporosis is thought to be a type of autoimmune disease.”
Stress
The inflammatory cytokines of the immune system, specifically IL-1 and IL-6, can cause calcium to be pulled from bone. When we are under stress, our stress hormone, cortisol, is secreted. Cortisol release signals the T-helper-2 cells to secrete IL-1 and IL-6. As well, when cortisol levels go up, our anti-aging and immune regulating hormone, DHEA, decreases. The body is designed to deal with short-term stressors, but when they become a regular occurrence, the connection between cortisol and IL-1/IL-6 causes bone to break down faster than it can be rebuilt.
Overactive Immune System
Osteoporosis may also be influenced by an overactive immune system. When macrophages (mobile white blood cells) overcome and consume the body’s invaders in the course of their daily surveillance, they release nitric oxide and IL-1. Nitric oxide in small amounts protects against bone loss. But when the immune system is fighting infection, macrophages release nitric oxide in large amounts, promoting the breakdown of bone. The drug Fosamax is designed to reduce nitric oxide, although with some terrible side effects. As mentioned earlier, IL-1 also promotes bone loss, so not only does vitamin D have to be available to control the secretion of IL-1, but macrophages have to be kept in balance as well. Nitric oxide, like vitamin D, is key to regulating bone.
Low Estrogen
Estrogen protects the body from excessive secretion of IL-1 and IL-6. Women with adrenal exhaustion, who have had hysterectomies, or top-level athletes with suppressed menses may all exhibit a lack of healthy estrogen associated with abnormally high levels of IL-1 (which promotes bone loss) and low levels of interferon gamma (which prevents bone loss).
Low Thyroid
The thyroid hormone thyroxin activates bone breakdown, so long-term elevated levels of the hormone for a prolonged period, either through hyperthyroidism or over-medication for hypothyroidism, results in bone loss. Sub-clinical low thyroid function, where not enough thyroid hormone is available, also promotes bone loss.
Medications
Use of medications may also contribute to osteoporosis: corticosteroid drugs decrease absorption of calcium, and antidepressants have been linked to increased risk of hip fractures. Drugs such as diuretics, antacids/PPIs, anti-convulsants, warfarin and lithium can also contribute to bone weakening.
Other Contributors
Other factors promoting osteoporosis include genetic predisposition (Asians and Caucasians are at higher risk), hyperparathyroidism, hypothyroidism, excessive alcohol consumption, leanness, never being pregnant, side effects of prescription medication, immobility or lack of exercise, and not getting enough sunlight. Smoking increases inflammatory immune factors promoting bone loss.
Major risk factors for osteoporosis:
- Corticosteroid therapy (prednisone)
- Depo-Provera (the birth control shot)
- Early menopause
- Excessive amounts of exercise
- Family history
- High alcohol intake
- High caffeine and sugar intake
- High-protein diet
- High-stress lifestyle or type A personality
- No pregnancies
- Northern European or Asian descent
- Sedentary lifestyle
- Suffering amenorrhea
- Thin or small build
- Use of proton pump inhibitors
Prescription for Bone Health
Diet
- Add nuts, seeds, and seaweed to diet to increase trace mineral intake.
- Avoid processed foods, refined carbohydrates, sugars, soft drinks, and limit dining out at restaurants.
- Avoid sources of poor-quality saturated fats such as deep-fried foods (chips, crackers, doughnuts), margarine, poor-quality oils (canola, safflower, sunflower, peanut and soy oils), hydrogenated and trans fats. Instead include grass-fed butter or ghee, as well as avocado, borage, coconut, extra virgin, and flax oils.
- Consume calcium-rich foods including canned salmon with the bones, broccoli, sesame and sunflower seeds, dark leafy vegetables, organic cheese and yogurt.
- Cook from scratch and use whole, fresh, and organic foods whenever possible.
- Cook with bone and vegetable stocks.
- Get enough protein, but not too much. Around 40 g for women (average body weight of 138 lbs), 63 g for men (average body weight of 174 lbs). Too much protein depletes calcium from the bones; too little prevents the formation of collagen and associated enzymes. Reduce animal protein by opting for vegetable-based protein such as legumes and add regular servings of fishes such as salmon, herring or mackerel.
- Include whole grains such as teff, buckwheat, amaranth, quinoa, millet, oats, and brown rice as they are a source of magnesium.
- Take calcium supplements before bed with a glass of orange juice. The blood calcium level is lower at night, so the rate of calcium absorption is greater.
- Whole grains, nut, and legumes should be soaked before use to break down phytic acid. When phytic acid is present in food it hinders the absorption of minerals.
Lifestyle
Develop an adequate exercise program that includes weight-bearing activities such as walking, hiking, stair climbing, dancing, weight training, jogging, skiing or low-impact aerobics. However, while regular movement and exercise is required to preserve bone mass and increase bone mineral density, excessive exercising can also lead to osteoporosis if food intake is not sufficient, menses are suppressed, or the immune system is hyper-stimulated.
Maintaining a healthy weight is important in preventing osteoporosis. Being too thin and not eating enough foods rich in bone building nutrients can contribute to the loss of bone density. It is especially important that athletes and those who exercise often are consuming enough food to protect bone health. In the past it was thought that obesity may be protective of bone health, new research now suggests that it actually increases the chances of weak bones.
Exposure to cigarette smoke and excess alcohol intake can increase chances of osteoporosis and should be avoided.
Supplements
Vitamin D is essential for the absorption of calcium into bone, and the skin is capable of producing this vitamin when exposed to sunlight for about 20 minutes per day. This is a problem during the winter months when there is less sunlight and many remain indoors. A Swiss study showed that supplementing with vitamin D helped reduce the risk of falls for the elderly. Magnesium is essential to convert vitamin D to its active form, and yet magnesium deficiency is common in the elderly population as well as in those with osteoporosis. Symptoms of magnesium deficiency include muscle cramps and twitching eyelids.
Calcium to Magnesium Ratio: Research has shown that the body requires twice as much calcium as magnesium. Taking more magnesium than calcium can actually suppress calcium levels and increase bone loss by decreasing the production of the thyroid hormone calcitonin. Magnesium in excess acts as a calcium blocker. There are times when extra magnesium can help; e.g., for restless leg syndrome, constipation, painful periods or heart palpitations, but for these, magnesium should be taken in divided doses and at a different time than a calcium supplement.
Generally, most people wait far too long to take bone-building nutrients. Most women do not start taking calcium until the age of 50. Young women need calcium, especially during the crucial bone-building years from ages 12 to 25.
| Nutrient | Dosage | Action |
|---|---|---|
| Multivitamin with minerals (contains no iron) |
Look for one that includes special bone nutrients:
Elemental calcium (glycinate/aspartate) 1000 mg Elemental magnesium (bisglycinate) 500 mg Vitamin D3 1000 IU Silicon 4 mg |
Ensures adequate nutrient status; contains all the bone nutrients needed to prevent and treat osteoporosis |
| Choline-stabilized orthosilicic acid | 10 mg | Important for the formation of collagen in bone
Research showed a 2% increase in bone strength over 12 months |
| Vitamin K2 MK7 | 100 mcg | Enhances osteocalcin, important for bone mineralization and increased bone strength |
| Natural Eggshell Membrane (NEM) | 500 mg | Relieves pain and stiffness in 7 days; helps rebuild cartilage |
| Vitamin D3 Activated Vitamin D3 |
1000 IU daily | Helps with thyroid function and calcium absorption |
| Omega-3 Fatty Acids | 750 mg of DHA and 500 mg of EPA |
Inhibits inflammatory IL-1, IL-6 and proinflammatory prostaglandins, known to promote calcium loss |
Health Tips to Enhance Healing
- Avoid antacids – they lower the acid in the gut and inhibit the absorption of calcium.
- Consume calcium-rich foods.
- Develop an adequate exercise program that includes weight-bearing activities
- Diets high in “good fats” enhance bone density. High-saturated-fat diets promote bone loss.
- Don’t wait till later in life to start consuming or supplementing bone supporting nutrients.
- Eat plenty of green leafy vegetables; they contain vitamin K, needed for proper bone mineralization.
- Eliminate all soft drinks; they lower calcium levels and increase phosphate levels.
- Include fermented soy in the diet from tempeh, miso, fermented soy powders and soy sauce.
- Maintain a balanced daily intake of protein.
- Quit smoking.
- Reduce consumption of caffeine (depletes calcium and magnesium), simple or refined sugars (also depletes calcium and lowers bone density), and alcohol (can lower vitamin D metabolism).
- Reduce salt; it increases calcium loss.
- Medication risk factors should be reviewed with a physician. Prednisone, Depo-Provera, steroids, blood thinners and diuretics are examples of drugs that increase risk of osteoporosis, yet a more natural approach may be taken. In some cases, a drug could be replaced with one with a lesser risk.
- Rule out hydrochloric acid deficiency. Low stomach acid impairs calcium absorption.
- See Arthritis
- See Menopause
- Take advantage of sunny days when possible and get at least 15 to 20 minutes of sunshine each day.